International Panel Defines Generalized Pustular Psoriasis for Clinical and Research Use
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of The Dermatologist or HMP Global, their employees, and affiliates.
International Panel Defines Generalized Pustular Psoriasis for Clinical and Research Use
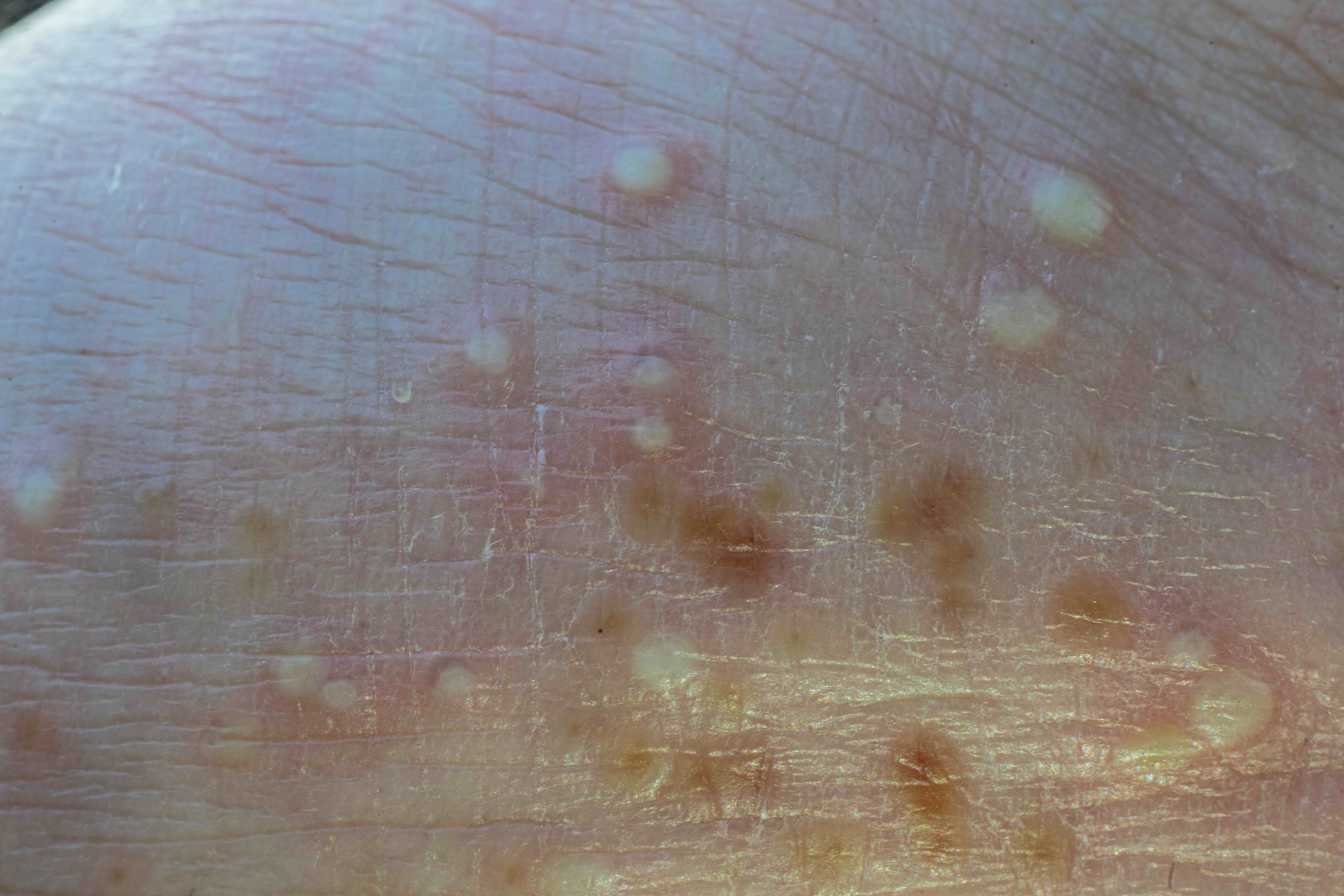 An international panel of dermatology experts has achieved consensus on a standardized definition and diagnostic criteria for generalized pustular psoriasis (GPP), a rare but serious systemic inflammatory skin disorder. The effort, published in JAMA Dermatology, aimed to reduce diagnostic delays and improve comparability in global research on GPP, which has previously lacked universally accepted clinical parameters.
An international panel of dermatology experts has achieved consensus on a standardized definition and diagnostic criteria for generalized pustular psoriasis (GPP), a rare but serious systemic inflammatory skin disorder. The effort, published in JAMA Dermatology, aimed to reduce diagnostic delays and improve comparability in global research on GPP, which has previously lacked universally accepted clinical parameters.
Using a modified Delphi method, the expert panel reviewed 64 challenging cases of GPP to generate 43 foundational statements addressing diagnostic features. These were refined and voted on during 2 virtual meetings involving 33 global experts. Consensus was defined as at least 80% agreement among participants.
In the first round, consensus was reached for 53% of statements, resulting in 23 accepted statements. The second round led to the final consensus definition: “Generalized pustular psoriasis is a systemic inflammatory disease characterized by cutaneous erythema and macroscopically visible sterile pustules.” The definition emphasizes that GPP can present with or without systemic symptoms, laboratory abnormalities, or coexisting psoriasis vulgaris.
The panel agreed on the following key diagnostic feature of GPP: “Macroscopically visible sterile pustules on [an] erythematous base and not restricted to the acral region or within psoriatic plaques.” They also distinguished between acute and subacute presentations, noting that GPP may appear as a sudden eruption of widespread pustules or present more gradually with annular patterns.
“These criteria represent a critical step forward in standardizing the diagnosis of GPP,” the authors noted. “They provide a foundation for more accurate diagnosis, better patient care, and enhanced comparability across clinical studies.”
Reference
Choon SE, van de Kerkhof P, Gudjonsson JE, et al. International consensus definition and diagnostic criteria for generalized pustular psoriasis from the International Psoriasis Council. JAMA Dermatol. 2024;160(7):758-768. doi:10.1001/jamadermatol.2024.0915
Nonsegmental Vitiligo: Combination Therapy With Ritlecitinib and Narrow-Band UVB
 A new exploratory analysis of a phase 2b extension study published in the Journal of the American Academy of Dermatology provides new insights into the efficacy and tolerability of combining oral ritlecitinib with narrow-band UVB (nbUVB) phototherapy in adults with nonsegmental vitiligo (NSV).
A new exploratory analysis of a phase 2b extension study published in the Journal of the American Academy of Dermatology provides new insights into the efficacy and tolerability of combining oral ritlecitinib with narrow-band UVB (nbUVB) phototherapy in adults with nonsegmental vitiligo (NSV).
In this extension study, 43 patients received ritlecitinib 200/ 50 mg with nbUVB twice weekly, while 187 received ritlecitinib monotherapy. Patients in the nbUVB arm were subject to a discontinuation criterion at week 12 if they failed to achieve at least 10% improvement in the Total Vitiligo Area Scoring Index (T-VASI).
At week 24 of the extension, efficacy was evaluated using both observed case (OC) and last observation carried forward analyses. The OC analysis demonstrated a statistically significant improvement in Facial Vitiligo Area Scoring Index (F-VASI) scores for the combination group vs monotherapy, with a mean percent change from baseline of -69.6% vs -55.1% (P = .009). Among patients with facial body surface area involvement ≥ 0.5%, 80.0% achieved at least F-VASI75 with combination therapy compared to 32.4% on monotherapy (OC; P = .007). For total body repigmentation, OC analysis showed a -46.8% change in T-VASI scores for ritlecitinib plus nbUVB vs -24.5% with monotherapy (P < .001). Half of the patients on combination therapy reached T-VASI50 vs 15.2% on monotherapy (P < .001).
In the OC analysis, 57.7% of patients receiving combination therapy reported being “much” or “very much” improved, compared to 30.0% on monotherapy (P = .012).
Safety profiles were generally favorable. Adverse events occurred in 74.4% of the combination group and 63.6% of the monotherapy group. Most adverse events were mild or moderate in both arms. Photosensitivity reactions (7.0%) and elevated creatine phosphokinase (9.3%) were more frequent with nbUVB.
Reference
Yamaguchi Y, Peeva E, Adiri R, et al. Response to ritlecitinib with or without narrow-band ultraviolet B add-on therapy in patients with active nonsegmental vitiligo: results from a phase 2b extension study. J Am Acad Dermatol. 2025;92(4):781-789. doi:10.1016/j.jaad.2024.11.064
Meta-Review Highlights Prevalence and Psychological Burden of Psoriatic Arthritis
 A recent overview of systematic reviews published in Rheumatology International consolidated existing data on the global prevalence, incidence, and psychological comorbidities associated with psoriatic arthritis (PsA), offering dermatologists a clearer picture of its epidemiologic footprint and emotional toll.
A recent overview of systematic reviews published in Rheumatology International consolidated existing data on the global prevalence, incidence, and psychological comorbidities associated with psoriatic arthritis (PsA), offering dermatologists a clearer picture of its epidemiologic footprint and emotional toll.
According to the analysis, which followed the Preferred Reporting Items for Overviews of Reviews, or PRIOR, guidelines, PsA remains a significant burden both in the general population and among patients with psoriasis. The pooled prevalence of PsA was estimated to range from 0.13% to 0.15% in the general population and from 15.5% to 19.7% in individuals with psoriasis.
The study also reported incidence rates ranging from 8.26 to 9.27 cases per 100,000 inhabitants annually in general populations. Notably, individuals with hidradenitis suppurativa had a reported PsA incidence of 0.87 cases, highlighting cross-condition relevance.
In addition to prevalence and incidence, the overview highlighted the psychological comorbidities that accompany PsA. Pooled prevalence rates were found to be 11.9% to 20% for depression, 19% to 33% for anxiety, 38% for alexithymia, and 72.9% for poor sleep quality. The incidence of depression in patients with PsA was also quantified, with a rate of 21.3 per 1,000 person-years.
"Depression and anxiety symptoms may be present in some patients with PsA," the authors stated, pointing to the need for psychosocial screening in clinical practice.
Importantly, the study uncovered geographic disparities in epidemiological data, suggesting variation in PsA burden by continent. Methodological inconsistencies were also identified in the existing literature, with several systematic reviews showing poor reporting across key A MeaSurement Tool to Assess systematic Reviews, or AMSTAR-2, items.
The authors concluded that “PsA seems to be prevalent and incident not only in people with psoriasis, but also in [the] general population.”
Reference
Hernández-Rodríguez JC, Infante-Cano M, García-Muñoz C, Matias-Soto J, Martinez-Calderon J. Psoriatic arthritis with psychological comorbidities: an overview of systematic reviews on incidence, prevalence, and geographic disparities. Rheumatol Int. 2024;44(11):2337-2355. doi:10.1007/s00296-024-05617-1
Premenstrual Flares in Atopic Dermatitis Recognized but Understudied
 Asystematic review published in Clinical and Experimental Dermatology has confirmed a consistent pattern of atopic dermatitis (AD) exacerbation in the premenstrual phase of the menstrual cycle, highlighting a gap in evidence-based treatment approaches for this subgroup of patients.
Asystematic review published in Clinical and Experimental Dermatology has confirmed a consistent pattern of atopic dermatitis (AD) exacerbation in the premenstrual phase of the menstrual cycle, highlighting a gap in evidence-based treatment approaches for this subgroup of patients.
Conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses, or PRISMA, guidelines, the review analyzed 16 publications across the Ovid Medline, Embase, Cochrane Library, PubMed, and Web of Science databases, finding that premenstrual flares of AD are widely acknowledged but poorly studied in terms of management strategies.
“All articles consistently acknowledged premenstrual deterioration in control of atopic dermatitis, typically occurring in the week prior to menstruation,” the authors reported.
Despite the uniformity of the findings regarding symptom timing, the review revealed a significant deficiency in data regarding potential interventions. “Existing studies are of a low quality, and we identified minimal evidence on treatment strategies for premenstrual AD exacerbations,” the authors wrote.
The authors called for future studies to address this gap, with a focus on developing therapeutic options that take hormonal modulation into account. “Further large-scale studies are needed to explore treatment options for these patients, such as hormonal therapies,” they concluded.
Reference
McSwiney NT, Hutchison E, Moran R, Phillips A, Sumra D, Wainman H. The impact of the menstrual cycle on exacerbations of atopic dermatitis: a systematic review. Clin Exp Dermatol. 2025:llaf153. doi:10.1093/ced/llaf153