AAD and NPF Issue Two New Psoriasis Guidelines
The American Academy of Dermatology and National Psoriasis Foundation have released 2 joint guidelines for the management and treatment of psoriasis.1,2
Based on current available evidence, the new guidelines are the first 2 of a series of 6 psoriasis guidelines to be released this year.3
One set of guidelines addresses common extracutaneous manifestations associated with psoriasis, including psoriatic arthritis, cardiovascular disease, metabolic syndrome, mental health conditions, and inflammatory bowel disease, and how the presence of these comorbidities can affect management of a patient’s psoriasis.1
The second set of guidelines discusses the treatment of psoriasis using biologics, including:
- Tumor necrosis factor alpha inhibitors, such as etanercept, infliximab, adalimumab, and certolizumab.
- IL-12/IL-23 inhibitors, such as ustekinumab.
- IL-17 inhibitors, such as secukinumab, ixekizumab, and brodalumab.
- IL-23 inhibitors, such as guselkumab, tildrakizumab, and risankizumab.2
“We believe this guideline will be a vital resource in the treatment of psoriasis,” said board-certified dermatologist Craig A. Elmets, MD, FAAD, co-chair of the work group that constructed the guidelines, in a press release.3
“Doctors should be aware of the conditions associated with this disease, educate patients accordingly, and work with those patients and other physicians to ensure that each patient receives the appropriate screening and treatment,” Dr Elmets said.3
References:
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities [published online February 13, 2019]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.11.058
- Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics [published online February 13, 2019]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.11.057
- Two new psoriasis guidelines address comorbidities, biologic treatment [press release]. Rosemont, IL: American Academy of Dermatology; February 13, 2019. https://www.aad.org/media/news-releases/two-new-psoriasis-guidelines-comorbidities-and-biologics. Accessed February 13, 2019.
Is Hyperhidrosis Tied to Psychiatric Health?
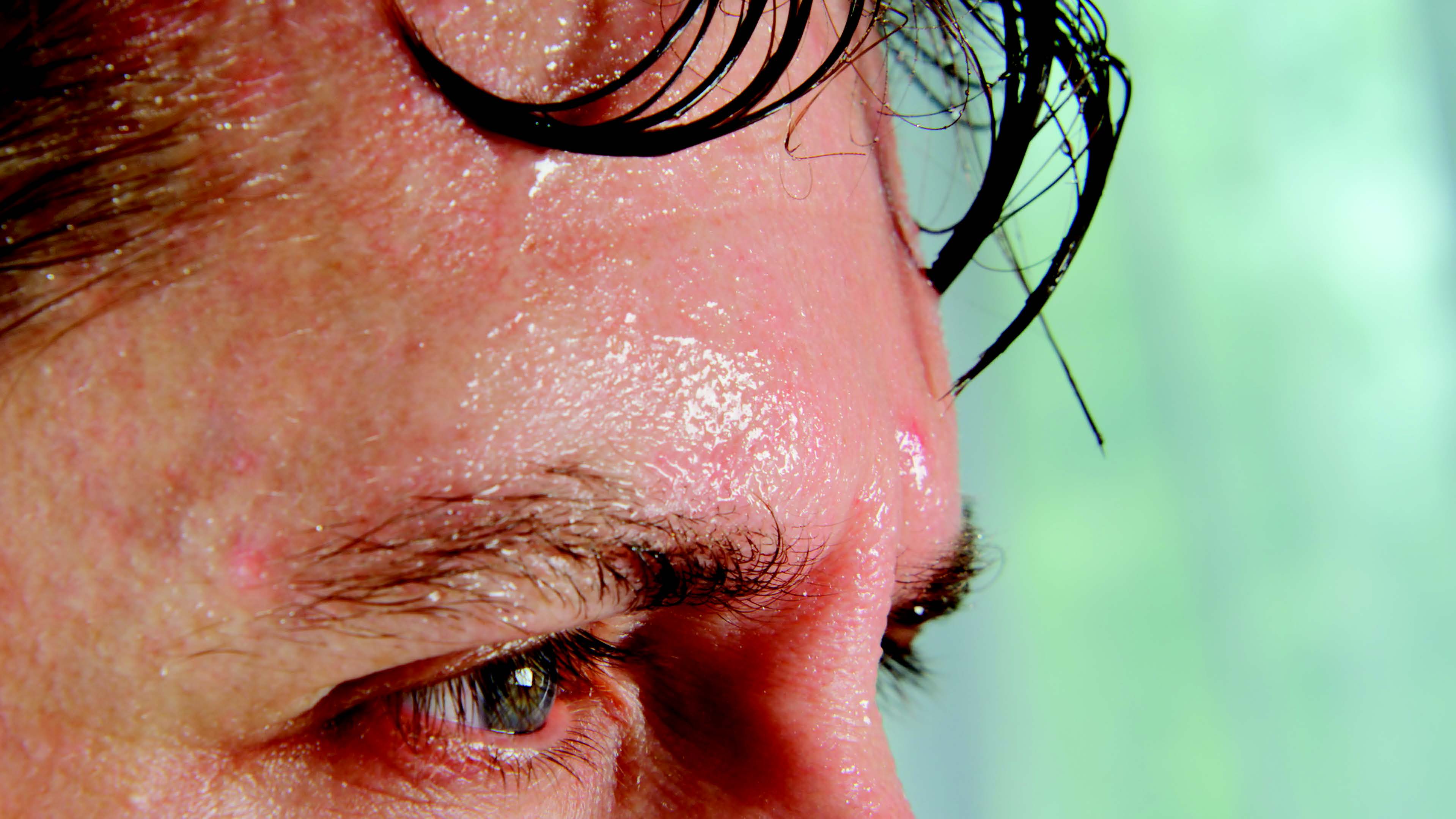 Patients with hyperhidrosis may be more likely to have certain psychiatric disorders than the general population, according to new findings presented at the 2019 American Academy of Dermatology Annual Meeting.
Patients with hyperhidrosis may be more likely to have certain psychiatric disorders than the general population, according to new findings presented at the 2019 American Academy of Dermatology Annual Meeting.
In a study of 500 participants with hyperhidrosis, researchers found that approximately 13.8% of participants had anxiety, while 12.4% had depression, and 6.4% had attention deficit disorder.
“We need to proactively ask our patients with hyperhidrosis if they suffer with or have symptoms of anxiety, depression or ADD,” said Dee Anna Glaser, MD, FAAD, professor, interim chair and director of clinical research and aesthetic and laser surgery in the department of dermatology at St. Louis University School of Medicine, in a press release. “We can let them know that’s pretty common and help them find care from the appropriate professionals.”
The study findings also demonstrated a correlation between mental health conditions and the number of body locations affected, but not for hyperhidrosis severity or body location. Further research will be needed to clarify the association of hyperhidrosis with mental health conditions.
Hyperhidrosis most commonly develops among adolescents and young adults, who can be especially prone to developing mental health conditions such as depression and anxiety, Dr Glaser noted. However, uncovering a potential association between hyperhidrosis and ADD was a surprising finding, she said.
“I think we need to look into that more and connect with individuals who have experience with ADD and together understand what that link may be,” said Dr Glaser in a press release.
Reference:
Research suggests connection between excessive sweating and mental health conditions [press release]. Washington, DC: American Academy of Dermatology; March 1, 2019. Accessed March 1, 2019. https://www.aad.org/media/news-releases/ hyperhidrosis-and-mental-health.
“Green Nail” in Imaging a Potential Sign for PsA
Indocyanine green-enhanced fluorescence optical imaging of the hands identified signals in patients’ nails that were highly specific for psoriatic arthritis (PsA), according to a study published in the Journal of the German Society of Dermatology.
“Early diagnosis of PsA poses a particular challenge,” the researchers wrote. “A novel fluorescence optical imaging technique, the Xiralite system, is very useful in this regard as it allows for visualization of microvasculature and perfusion.”
Researchers described a pair of investigations. In the first, they analyzed extra-articular fluorescence optical signal patterns in 241 imaging sequences from 187 participants with PsA and compared them with 36 fluorescence optical sequences from 31 participants with rheumatoid arthritis, who served as a control group. In a follow-up analysis, they evaluated 203 consecutive fluorescence optical sequences from 54 participants with PsA and 149 control subjects with various inflammatory rheumatic disorders to validate patterns identified in the primary study.
Participants with PsA demonstrated 3 different fluorescence optical signal patterns in the nails, according to the study. One pattern, called the “green nail” sign, was 97% specific for PsA in the first analysis and 87% specific for PsA in the follow-up analysis compared with controls.
“The ‘green nail’ phenomenon seems to be of particular diagnostic interest as a potential sign of impaired microcirculation of the nail bed,” the researchers wrote.
Reference:
Wiemann O, Werner SG, Langer HE, Backhaus M, Chatelain R. The "green nail" phenomenon in ICG-enhanced fluorescence optical imaging—a potential tool for the differential diagnosis of psoriatic arthritis. J Dtsch Dermatol Ges. 2019;17(2):138- 147. doi:10.1111/ddg.1347
Hidradenitis Suppurativa Associated With Lymphoma Risk
Patients with hidradenitis suppurativa (HS) have 2 to 4 times higher odds of developing lymphomas compared with the general population, according to the findings of a recent research letter.
In the study, the researchers identified 62,690 patients with HS and 28,937,880 controls using standardized electronic health record information from the IBM Explorys database. They assessed the overall prevalence of non-Hodgkin lymphoma (NHL), Hodgkin disease (HL), and primary cutaneous T-cell lymphoma (CTCL) among individuals with and without HS.
The crude prevalences of NHL, HL, and CTCL among individuals with HS were 0.40%, 0.17%, and 0.06% compared with 0.35%, 0.09%, and 0.02% among those without HS, respectively.
Multivariable analyses showed that individuals with HS had increased overall odds of developing NHL (odds ratio [OR], 2.0), HL (OR, 2.21), and CTCL (OR, 4.31). Compared with women with HS, men with HS had higher prevalences of NHL, HL, and CTCL.
Individuals with HS aged 65 years and older had higher prevalences of NHL and CTCL compared with those aged 45 to 64 years and those aged 18 to 44 years. The prevalence of NHL was 1.2%, 0.52%, and 0.20% for individuals aged 65 years or older, those aged 45 to 64 years, and those aged 18 to 44 years, respectively. Likewise, the prevalence of CTCL was 0.17%, 0.07%, and 0.03% for individuals aged 65 years or older, those aged 45 to 64 years, and those aged 18 to 44 years, respectively.
Compared with individuals without HS aged 18 to 44 years, those with HS between 18 and 44 years had a 3.64 higher odds of developing NHL. Similarly, individuals with HS in the 45 to 64 year age group and 65 years or older age group had 1.99 higher odds of NHL compared with those without HS in the same age groups.
“Patients with HS have malignant lymphomas more frequently than the general population,” the researchers concluded.
Reference:
Tannenbaum R, Strunk A, Garg A. Association between hidradenitis suppurativa and lymphoma [Published online January 30, 2019]. JAMA Dermatol. doi:10.1001/ jamadermatol.2018.5230



















