What’s New in Allergic Contact Dermatitis? 2025’s Allergens on the Rise
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of The Dermatologist or HMP Global, their employees, and affiliates.
The diagnosis and/or management of allergic contact dermatitis (ACD) currently accounts for 4% to 7% of general dermatology visits annually.1 This delayed-type hypersensitivity reaction to exogenous agents may affect up to 20% of the general population.2 ACD can be diagnosed when a patient presents with a new, localized eczematous dermatitis in combination with a positive exposure history. Patch testing, the widely accepted gold standard diagnostic tool, can also be used to make the diagnosis.3
The allergens commonly implicated in ACD are vast and numerous, including preservatives, emulsifiers, fragrances, medicaments, metals, rubber accelerators, and textile dyes.4 Many of these allergens are often reflected in the modernization of today’s world, which has led to increased occupational, consumer, and iatrogenic exposures. Further complicating this highly specialized field of dermatology is the dynamic nature of consumerism and the ever-changing personal care product trends found on various social media platforms.
The changing array of exposures can make it difficult to maintain a consistent understanding of the allergens associated with ACD. In this article, we discuss the up-and-coming allergens for 2025, their chemical function, their role in consumer products, and the reported cases of contact allergy. Given the high prevalence of ACD in the general population, dermatologists should be aware of these emerging allergens. Coupled with the right clinical scenario, detection of any of these ingredients when obtaining a product history from a patient may necessitate a patch testing referral.
Panthenol
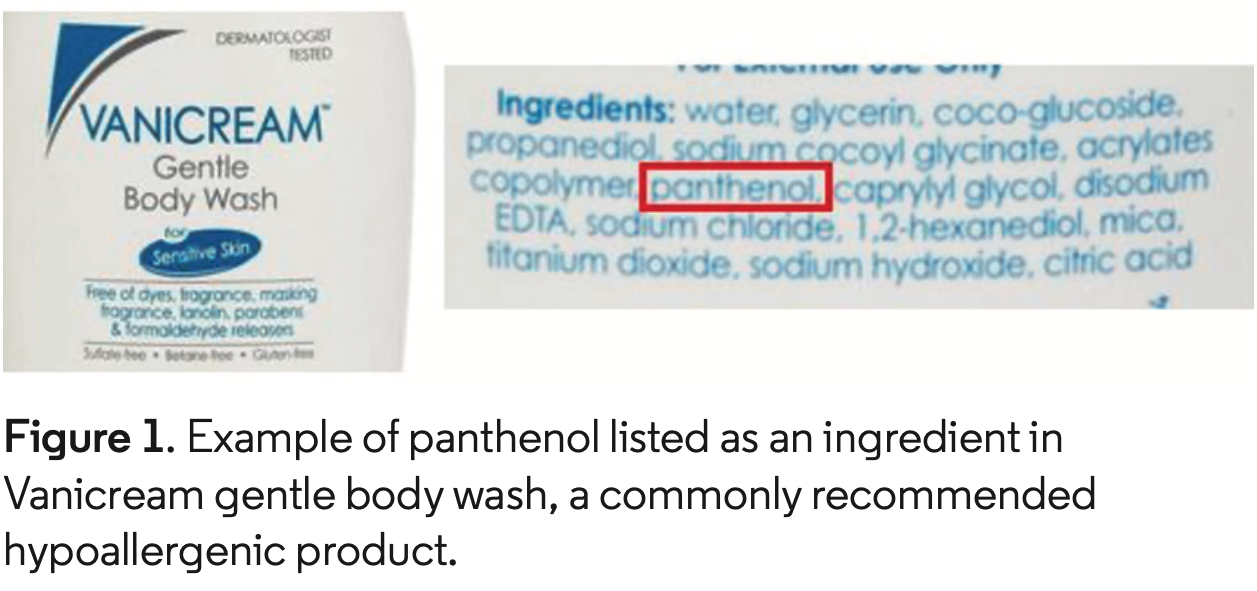 Panthenol is a vitamin B5 derivative that plays a key role in maintaining epithelial function through the synthesis of fatty acids in the stratum corneum.5 Panthenol decreases transepidermal water loss, improves epidermal hydration, and can modulate the expression of genes involved in wound healing.6,7 Over time, panthenol’s ability to act as a skin moisturizer/barrier restorer and wound healing agent has resulted in its frequent inclusion in consumer products, many of which are marketed as “hypoallergenic” or “gentle.” Products from widely recognized dermatologist-recommend brands commonly contain panthenol (Figure 1).8
Panthenol is a vitamin B5 derivative that plays a key role in maintaining epithelial function through the synthesis of fatty acids in the stratum corneum.5 Panthenol decreases transepidermal water loss, improves epidermal hydration, and can modulate the expression of genes involved in wound healing.6,7 Over time, panthenol’s ability to act as a skin moisturizer/barrier restorer and wound healing agent has resulted in its frequent inclusion in consumer products, many of which are marketed as “hypoallergenic” or “gentle.” Products from widely recognized dermatologist-recommend brands commonly contain panthenol (Figure 1).8
Twelve cases of ACD to panthenol have been reported, 5 of which involved reactions to “natural” or “hypoallergenic” products, and 4 of which were specifically linked to panthenolcontaining wound healing creams.8 Many of these cases began with initial positive reactions to personal products tested “as-is,” with subsequent testing of the individual ingredients revealing panthenol as the culprit allergen. At our specialized patch testing center, we have observed 13 reactions to panthenol over the last 4.5 years, 5 of which involved “hypoallergenic” personal care products and 7 of which were deemed to have definite or probable relevance.
Cetrimonium chloride and cetrimonium bromide
 Cetrimonium chloride and cetrimonium bromide belong to a class of chemicals called quaternary ammonium compounds.9 These allergens are cationic (positively charged), which allows them to penetrate and neutralize electrical charge on the hair surface. For this reason, they are frequently used in hair care products, especially shampoos/conditioners, styling gels, and detanglers (Figure 2). Cetrimonium chloride and cetrimonium bromide also have preservative and antiseptic qualities and are occasionally in cleaning and disinfecting products.10 Both allergens are related to and may cross react with a more well-known quaternary ammonium compound, benzalkonium chloride.
Cetrimonium chloride and cetrimonium bromide belong to a class of chemicals called quaternary ammonium compounds.9 These allergens are cationic (positively charged), which allows them to penetrate and neutralize electrical charge on the hair surface. For this reason, they are frequently used in hair care products, especially shampoos/conditioners, styling gels, and detanglers (Figure 2). Cetrimonium chloride and cetrimonium bromide also have preservative and antiseptic qualities and are occasionally in cleaning and disinfecting products.10 Both allergens are related to and may cross react with a more well-known quaternary ammonium compound, benzalkonium chloride.
There are few published reports detailing contact reactions to cetrimonium bromide and none discussing cetrimonium chloride. One recent study highlighted the potential for cetrimonium bromide-containing hair products to cause frontal fibrosing alopecia,11 and another concluded that this allergen is an up-and-coming cause of pigmented cosmetic dermatitis.12 Several case reports of ACD to cetrimide, which contains cetrimonium bromide, have been published, with most implicated products being antiseptic solutions.13 At our specialized patch testing center, we have observed 536 reactions to several concentrations of cetrimonium chloride over the last 4.5 years and 36 reactions to cetrimonium bromide, which we started testing to about 6 months ago.

Tacrolimus and pimecrolimus
Tacrolimus ointment and pimecrolimus cream are nonsteroidal anti-inflammatory medications that belong to a class of drugs known as topical calcineurin inhibitors. In the last several decades, both treatments have been increasingly utilized for a wide variety of dermatologic conditions (atopic dermatitis, periorificial dermatitis, contact dermatitis, seborrheic dermatitis, psoriasis) and they remain an alternative to topical corticosteroids given their minimal adverse reactions.14
There have been several cases of tacrolimus and/or pimecrolimus contact allergy published in the literature.15-19 Patients may be allergic to the active ingredient (tacrolimus or pimecrolimus) or one of the inactive ingredients present in these medicaments (Table). To delineate the culprit allergen, it is recommended to test both the commercial preparation of tacrolimus/pimecrolimus along with as many of its inactive ingredients as possible. There has also been reports of potential cross-reaction between these 2 medicaments, with patients demonstrating positive patch test reactions to both tacrolimus and pimecrolimus.20,21 At our institution, we have had 40 patient reactions to pimecrolimus and 6 patient reactions to tacrolimus over the last 4.5 years. The decision to test to these medicaments is based primarily on patient history.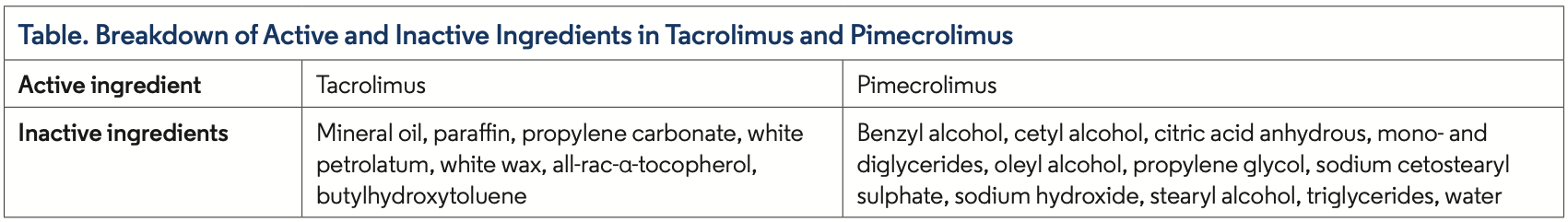
Chlorphenesin
Chlorphenesin is frequently incorporated into a variety of cosmetic and skin care products as an antimicrobial preservative. In the 1980s, initial cases of ACD were reported in patients using anti-fungal creams that contained chlorphenesin. Several additional cases of chlorphenesin-related ACD were published in the early 2000s, with culprit products including deodorants, moisturizers, foundations, and sunscreens.22 More recently, a case published in 2022 was linked to a moisturizing cream,22 and a case published in 2025 was linked to a topical emollient.23
Currently, there is no commercially available preparation to perform chlorphenesin patch testing; most cases have been identified through testing the individual ingredients of culprit products supplied by manufacturers. Several authors have commented on the possibility of chlorphenesin-related ACD being an “underdiagnosed and overlooked phenomenon,” further speculating on future increases in its incidence.22,23 Given its frequent use in cosmetics and skin care products, more routine testing to this allergen may be warranted. At our specialized patch testing center, we do not currently test to chlorphenesin but are making plans to do so soon.
Key Takeaways
Knowledge of emerging allergens can be useful when evaluating patients with suspected ACD and may even guide dermatology providers toward a patch testing referral. Below are the key insights that we believe are most important for dermatologists to take away from this article.
- Panthenol: This allergen is frequently found in “hypoallergenic” skin care products, many of which are dermatologist recommended for patients with suspected ACD. If a patient who transitions to these products fails to improve, they may benefit from patch testing, which should include panthenol.
- Cetrimonium chloride and cetrimonium bromide: These allergens are often found in hair care products. If a patient develops new onset dermatitis in a “rinse-off” distribution (scalp, face, neck, upper trunk) after trying a new hair care product, patch testing may be beneficial.
- Tacrolimus and pimecrolimus: If a patient using tacrolimus or pimecrolimus as a steroid alternative fails to improve or has worsening dermatitis in areas applied, patch testing to these medicaments may be warranted.
- Chlorphenesin: This allergen is being increasingly incorporated into cosmetics and skin care products, and reported cases are expected to rise in the future.
Brailyn Weber is a research fellow at Park Nicollet Contact Dermatitis Clinic in Minneapolis, MN, and a fourth-year medical student at the University of North Dakota School of Medicine in Grand Forks, ND. Dr Hylwa is the Allergen Focus section editor, a faculty physician in the department of dermatology at Hennepin Healthcare and Park Nicollet Contact Dermatitis Clinic, and an assistant professor at the University of Minnesota in Minneapolis, MN.
Disclosure: Dr Hylwa has received speaker honoraria from the Contact Dermatitis Institute and the Alabama Dermatologic Society.
References
- Tramontana M, Hansel K, Bianchi L, Sensini C, Malatesta N, Stingeni L. Advancing the understanding of allergic contact dermatitis: from pathophysiology to novel therapeutic approaches. Front Med (Lausanne). 2023;10:1184289. doi:10.3389/fmed.2023.1184289
- Alinaghi F, Bennike NH, Egeberg A, Thyssen JP, Johansen JD. Prevalence of contact allergy in the general population: a systematic review and meta-analysis. Contact Dermatitis. 2019;80(2):77-85. doi:10.1111/cod.13119
- Fonacier L. A practical guide to patch testing. J Allergy Clin Immunol Pract. 2015;3(5):669-675. doi:10.1016/j.jaip.2015.05.001
- Fonacier L, Frankel D, Mawhirt S. Contact allergens for the allergist. Ann Allergy Asthma Immunol. 2022;128(6):629-644. doi:10.1016/j.anai.2022.03.022
- Proksch E, de Bony R, Trapp S, Boudon S. Topical use of dexpanthenol: a 70th anniversary article. J Dermatolog Treat. 2017;28(8):766-773. doi:10.1080/0954663 4.2017.1325310
- Heise R, Skazik C, Marquardt Y, et al. Dexpanthenol modulates gene expression in skin wound healing in vivo. Skin Pharmacol Physiol. 2012;25(5):241-248. doi:10.1159/000341144
- Gehring W, Gloor M. Effect of topically applied dexpanthenol on epidermal barrier function and stratum corneum hydration. Results of a human in vivo study. Arzneimittelforschung. 2000;50(7):659-663. doi:10.1055/s-0031-1300268
- Weber B, Hylwa S. Panthenol allergic contact dermatitis: sources of exposure, reported cases, and a call for more frequent testing. Dermatitis. 2024 Dec 23. Online ahead of print. doi:10.1089/derm.2024.0489
- Arnold WA, Blum A, Branyan J, et al. Quaternary ammonium compounds: a chemical class of emerging concern. Environ Sci Technol. 2023;57(20):7645-7665. doi:10.1021/acs.est.2c08244
- Okeke CAV, Khanna R, Ehrlich A. Quaternary ammonium compounds and contact dermatitis: a review and considerations during the COVID-19 pandemic. Clin Cosmet Investig Dermatol. 2023;16:1721-1728. doi:10.2147/CCID.S410910
- Truel JS, Wang CX, Schlessinger DI, Sheinbein DM, Mann CM. Cetrimonium bromide patch test positivity is found with a high frequency in a cohort of patients with frontal fibrosing alopecia. Dermatitis. 2024;35(1):100-101. doi:10.1089/derm.2022.0086
- Sharma VK, Bhatia R, Yadav CP. Clinical profile and allergens in pigmented cosmetic dermatitis and allergic contact dermatitis to cosmetics in India. Dermatitis. 2018;29(5):264-269. doi:10.1097/DER.0000000000000407
- Lee JY, Wang BJ. Contact dermatitis caused by cetrimide in antiseptics. Contact Dermatitis. 1995;33(3):168-171. doi:10.1111/j.1600-0536.1995.tb00539.x
- Bubna AK. Topical tacrolimus and pimecrolimus in dermatology: an overview. Clin Dermatol Rev. 8(3):85-196. doi:10.4103/cdr.cdr_121_23
- Saitta P, Brancaccio R. Allergic contact dermatitis to pimecrolimus. Contact Dermatitis. 2007;56(1):43-44. doi:10.1111/j.1600-0536.2007.00822.x
- Xiong M, Hylwa S. Too much of a good thing? Allergic contact dermatitis to pimecrolimus. Dermatitis. 2022;33(6):e65-e66. doi:10.1097/ DER.0000000000000870
- Neczyporenko F, Blondeel A. Allergic contact dermatitis to Elidel cream itself? Contact Dermatitis. 2010;63(3):171-172. doi:10.1111/j.1600-0536.2010.01764.x 1
- Zhang AJ, Warshaw EM. Allergic contact dermatitis caused by mupirocin and pimecrolimus. Contact Dermatitis. 2019;80(2):132-133. doi:10.1111/cod.13142
- Shaw DW, Eichenfield LF, Shainhouse T, Maibach HI. Allergic contact dermatitis from tacrolimus. J Am Acad Dermatol. 2004;50(6):962-965. doi:10.1016/j. jaad.2003.09.013
- Shaw DW, Maibach HI, Eichenfield LF. Allergic contact dermatitis from pimecrolimus in a patient with tacrolimus allergy. J Am Acad Dermatol. 2007;56(2):342-345. doi:10.1016/j.jaad.2006.09.033
- Schmutz JL, Barbaud A, Tréchot P. Allergie de contact au tacrolimus puis au pimécrolimus [Contact allergy with tacrolimus then pimecrolimus]. Ann Dermatol Venereol. 2008;135(1):89. doi:10.1016/j.annder.2007.12.003
- Herman A, de Montjoye L, Baeck M. Re-emergence of allergic contact dermatitis from chlorphenesin. Contact Dermatitis. 2022;87(5):464-465. doi:10.1111/ cod.14196
- Moreira de Nogueira CM, Dias Cerqueira C, Santos Ribeiro MÂ, Marques Pereira Cabral Ribeiro TM. Chlorphenesin-induced allergic contact dermatitis: an overlooked phenomenon? Dermatitis. 2025 Jan 17. Online ahead of print. doi:10.1089/derm.2024.0433























