What Is This Painless Solid Mass on the Upper Eyelid?
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Dermatology Learning Network or HMP Global, their employees, and affiliates.
Case Report
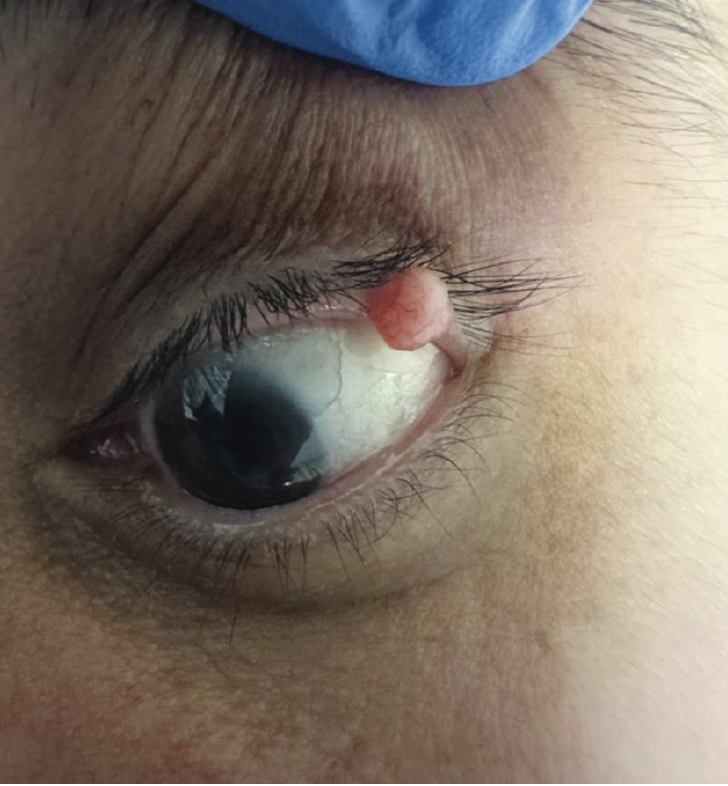
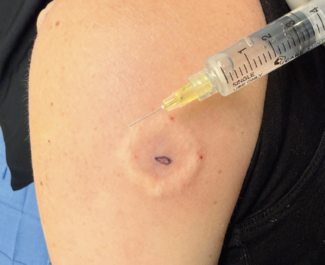
A 51-year-old man sought dermatologic evaluation for an asymptomatic, persistent growth on his left upper eyelid due to mild obstruction of vision (Figure 1). The lesion, evolving over the course of 3 years, exhibited slow, gradual growth and minor discomfort without the presence of pain or itching. Upon examination, a solitary, flesh-colored 8-mm x 7-mm papule without scale, ulceration, or crust was identified on the left upper eyelid, extending to the mucosal surface. A partial shave biopsy was performed.
What is your diagnosis?
Check your answer below
Diagnosis
Palisaded Encapsulated Neuroma
Palisaded encapsulated neuroma (PEN), also called solitary circumscribed neuroma, is a rare benign cutaneous neural tumor that commonly occurs in adults aged 40 to 60 years, with a female to male ratio of 1:1.1,2 Lesions are typically slow-growing, asymptomatic, solitary, flesh-colored nodules. In certain cases, PEN may present with multiple lesions.1 The anatomic distribution of PEN is typically confined to regions adjacent to mucocutaneous junctions, primarily found on the face, with a few rare exceptions, including the oral cavity, shoulder, trunk, and extremities.2 Infrequently, it has been reported to involve the eyelid.3,4
Clinical Presentation
PEN classically presents as a skin-colored papule or nodule ranging from 2 mm to 6 mm near mucocutaneous junctions and on the head and neck.2 PEN predominantly features a solitary, nodular growth pattern.5 Unusual and uncommon variants of PEN include plexiform and multinodular. Plexiform neuroma is a particularly important variant due to its association with von Recklinghausen disease and risk of malignant transformation.5 Rarely, PEN may present with multiple lesions.1 Multinodular PEN is unique because cases with these lesions present with multiple tumor nodules of various sizes arranged in a perpendicular manner.5
PEN may mimic cutaneous neurofibroma, melanocytic nevus, or cutaneous schwannoma, thus histologic analysis is crucial in differentiating PEN.1 Ophthalmologists may overlook PEN due to a lack of familiarity with the condition.4 Given that PEN typically presents as a harmless, solitary growth without any relationship with systemic syndromes and infrequent recurrence, it is important to differentiate it from tumors like basal cell carcinoma (BCC) or other neural tumors that require comprehensive systemic evaluation.3 Pathologists must be mindful of the presence of plexiform and multinodular variants of PEN to prevent misdiagnosis as a plexiform neurofibroma or schwannoma.6
Association With Other Syndromes
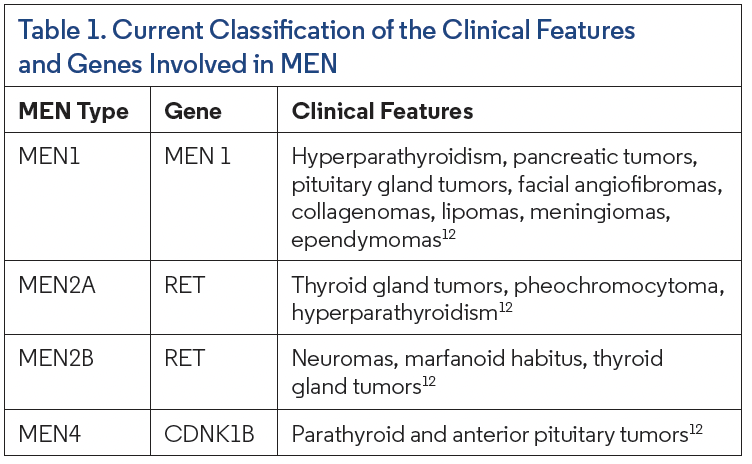
While PEN is a benign neural tumor with limited literature associating it with systemic syndromes, rare cases of multiple cutaneous PENs have been documented in adult patients both with and without features of multiple endocrine neoplasia, type 2B (MEN 2B).7-9 Misago et al. discussed the observation of hybrid MEN 2B-type neuromas and PEN with MEN 2B neuromas, noting that PEN may be a characteristic finding in cases of multiple mucocutaneous neuromas.9 Multiple mucosal neuromas in MEN 2B, a rare syndrome with potentially fatal clinical consequences, may appear similarly to PEN as a nonpainful papule on the lips, tongue, buccal mucosa, and oral cavity (Table 1).10,11
Differential Diagnosis
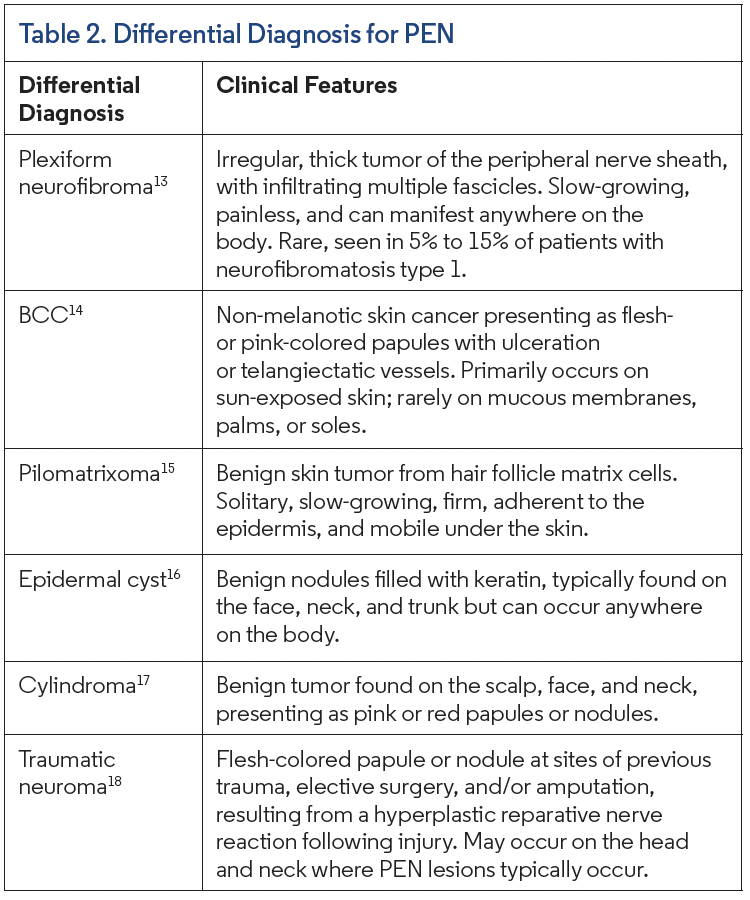
Distinguishing PEN presents a challenging task due to the overlap in clinical features with various other diseases. The differential diagnosis encompasses conditions such as plexiform neurofibroma, BCC, pilomatrixoma, epidermal cyst, and cylindroma (Table 2).13-18
Management
PEN is frequently misdiagnosed, thus accurate clinical diagnosis with histologic analysis may improve patient prognosis and ensure excision without recurrence.19 Once identified clinically and histologically, lesions can be excised with ease without recurrence.19 The treatment of PEN typically involves conservative local surgical excision.19 In certain cases, the initial biopsy of the lesion removes the entire tumor and additional excision is not required. Recurrence following biopsy and excision is rare.20 In cases where local recurrence was seen, there was no subsequent recurrence upon re-excision.20
During excision, Reed et al. described the unveiling of a ball of tumor nestled within the dermis revealed as the epidermis and superficial dermis separated upon cutting into the lesion.21 This unique finding can assist in accurate diagnosis because a limited number of other tumors, a pilar cyst for example, present in this way. In cases of PEN, patients can be assured that excision is typically curative with a low likelihood of recurrence, reducing the necessity for additional testing or concern regarding development of systemic disease or malignancy.1 These compelling data underscore the effectiveness of excision as comprehensive treatment and its role in ensuring long-term success in managing PEN.
Our Patient
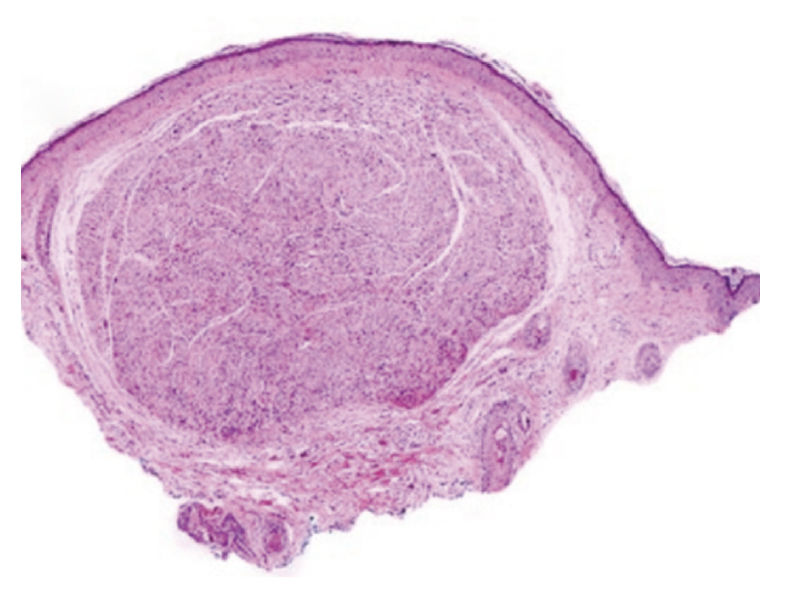
Upon evaluating the clinical presentation, a diagnosis of PEN was made, and histopathologic confirmation was established via a partial biopsy (Figure 2). Subsequently, the chosen course of treatment during the follow-up appointment involved surgical removal of the remaining lesion. At a 4-month follow up, the patient’s discomfort was resolved with no tumor recurrence.
Conclusion
PEN is a benign cutaneous neural tumor that commonly occurs on the head and neck of middle-aged adults as a slow-growing, asymptomatic, flesh-colored nodule. The potential for misdiagnosis arises due to the clinical presentation of PEN overlapping with that of other conditions, such as cutaneous schwannoma, neurofibroma, traumatic neuroma, and melanocytic nevus, posing a challenge for diagnostic accuracy. Correct diagnosis may also prevent unnecessary clinical concern and additional unnecessary testing for the patient. To circumvent these concerns, histologic analysis is crucial. While this benign neural tumor typically carries an excellent prognosis with low recurrence rates post-surgical excision, periodic clinical evaluations may be recommended to monitor for any signs of recurrence or associated symptoms. Facilitating timely and accurate treatment interventions may also prevent malignant transformation.
References
1. Batra J, Ramesh V, Molpariya A, Maan KK. Palisaded encapsulated neuroma: an unusual presentation. Indian Dermatol Online J. 2018;9(4):262-264. doi:10.4103/ idoj.IDOJ_354_17
2. Reed RJ, Fine RM, Meltzer HD. Palisaded, encapsulated neuromas of the skin. Arch Dermatol. 1972;106(6):865-870. doi:10.1001/archderm.1972.01620150051016
3. Dubovy SR, Clark BJ. Palisaded encapsulated neuroma (solitary circumscribed neuroma of skin) of the eyelid: report of two cases and review of the literature. Br J Ophthalmol. 2001;85(8):949-951. doi: 10.1136/bjo.85.8.949
4. Al-Holou SN, Hansen ED, Bermudez A, Fernandez MP, Dubovy SR. Palisaded encapsulated neuroma of the eyelid: clinicopathological correlation. Invest Ophthalmol Vis Sci. 2016;57(12):2414.
5. Argenyi ZB, Cooper PH, Santa Cruz D. Plexiform and other unusual variants of palisaded encapsulated neuroma. J Cutan Pathol. 1993;20(1):34-39. doi:10.1111/j.1600-0560.1993.tb01246.x
6. Leblebici C, Savli TC, Yeni B, Cin M, Aksu AEK. Palisaded encapsulated (solitary circumscribed) neuroma: a review of 30 cases. Int J Surg Pathol. 2019;27(5):506-514. doi:10.1177/1066896919833172
7. Moore RL, White CR. Multiple palisaded encapsulated neuromas in a child without other associated abnormalities. J Am Acad Dermatol. 2010;62(2):358-359. doi:10.1016/j.jaad.2009.01.036
8. Lee MS, Lee JD, Cho SH, Kim HS. Palisaded encapsulated neuroma in a zosteriform distribution. Indian J Dermatol. 2016;61(1):126. doi:10.4103/0019-5154.174173
9. Misago N, Toda S, Narisawa Y. The relationship between palisaded encapsulated neuroma and the mucocutaneous neuroma seen in multiple endocrine neoplasia 2b syndrome: a histopathologic and immunohistochemical study. Am J Dermatopathol. 2014;36(7):562-569. doi:10.1097/DAD.0000000000000021
10. Mortazavi N, Gholami A, Amini Shakib P, Hosseinkazemi H. Palisaded encapsulated neuroma of the tongue clinically imicking a pyogenic granuloma: a case report and review of literature. J Dent (Tehran). 2015;12(7):537-541.
11. Qualia CM, Brown MR, Ryan CK, Rossi TM. Oral mucosal neuromas leading to the diagnosis of multiple endocrine neoplasia type 2B in a child with intestinal pseudo-obstruction. Gastroenterol Hepatol (N Y). 2007;3(3):208-211.
12. Khatami, Fatemeh, Tavangar, Mohammad S. Multiple endocrine neoplasia syndromes from genetic and epigenetic perspectives. Biomarker Insights. 2018;13:117727191878512. doi:10.1177/1177271918785129
13. Poswal P, Bhutani N, Arora S, Kumar R. Plexiform neurofibroma with neurofibromatosis type I/von Recklinghausen’s disease: a rare case report. Ann Med Surg (Lond). 2020;57:346-350. doi:10.1016/j.amsu.2020.08.015
14. McDaniel B, Badri T, Steele RB. Basal cell carcinoma. In: StatPearls [Internet]. StatPearls Publishing; 2024.
15. Zhao A, Kedarisetty S, Arriola AGP, Isaacson G. Pilomatrixoma and its imitators. Ear Nose Throat J. 2024;103(3):183-189. doi:10.1177/01455613211044778
16. Zito PM, Scharf R. Epidermoid cyst. In: StatPearls [Internet]. StatPearls Publishing; 2023.
17. Khoury E, Godfrey M, Yeoh CC. Gynaecological cylindroma in association with CYLD gene mutation. Oxf Med Case Reports. 2022;2022(1):omab139. doi:10.1093/ omcr/omab139
18. Yang H, Dong Y, Wang Z, et al. Traumatic neuromas of peripheral nerves: diagnosis, management and future perspectives. Front Neurol. 2023;13:1039529. doi:10.3389/fneur.2022.1039529
19. Newman MD, Milgraum S. Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. Dermatol Online J. 2008;14(7):12.
20. Koutlas IG, Scheithauer BW. Palisaded encapsulated (“solitary circumscribed”) neuroma of the oral cavity: a review of 55 cases. Head Neck Pathol. 2010; 4(1):15-26. doi:10.1007/s12105-010-0162-x
21. Reed RJ, Fine RM, Meltzer HD. Palisaded, encapsulated neuromas of the skin. Arch Dermatol. 1972;106(5):865-870.