What Is This Hyperpigmented Annular Axillary Rash?

Case ReportAn otherwise healthy 56-year-old White woman presented to the dermatology department for evaluation of a rash to the bilateral axillae, wrists, and inframammary folds. The rash had been worsening over the past 3 months. No pertinent past medical history. Review of systems was negative. Lesions were mildly pruritic. Cutaneous examination revealed multiple hyperpigmented annular and polycyclic macules and patches with an elevated violaceous border in the bilateral axillary (Figure 1) and inframammary folds. In the same regions, the patient also had multiple scattered violaceous, flat-topped papules. On the volar aspects of the wrists, she also had multiple violaceous polygonal flat-topped papules. No nail changes or oral lesions were appreciated.
What Is This Hyperpigmented Annular Axillary Rash?

Diagnosis: Lichen Planus Pigmentosus Inversus
Lichen planus pigmentosus (LPP) is a less common and underreported variant of lichen planus (LP) that presents as hyperpigmented dark brown to gray macules and patches that may be mildly pruritic or asymptomatic.1 The affected areas are typically sun-exposed sites such as the face, neck, and upper extremities. However, involvement of the intertriginous and flexural areas has also been reported and is classified as lichen planus pigmentosus inversus (LPPI) (Figure 1). LPPI was first described by Pock et al in 2001 after the examination of both clinical and microscopic findings of seven patients with LPP affecting the intertriginous areas.1
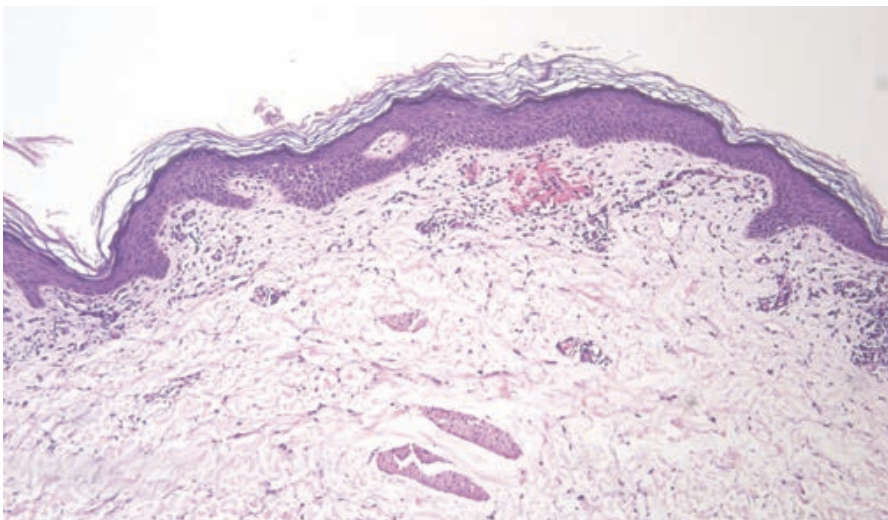
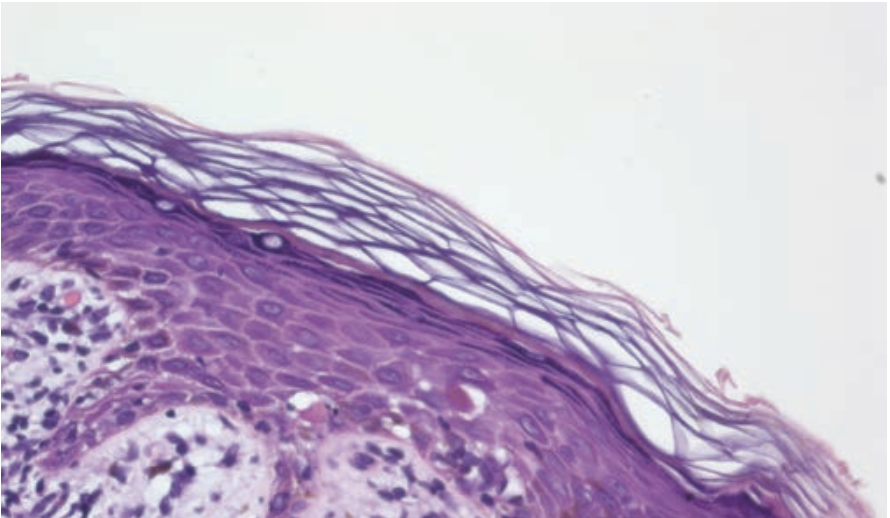
LPP may affect patients of all races but classically favors skin types III and IV. Patients are typically between the third and fifth decades of life and women are more commonly affected. As is true of classic LP, patients infected with hepatitis C virus may also be more prone to LPP. Endocrinopathies such as type 2 diabetes, thyroid disease, or dyslipidemia may also be associated.2 Triggers of LPP may include photosensitizing agents and sun exposure, or tight clothing or friction as commonly is the case in LPPI. Histologic examination may reveal an atrophic epidermis with hypergranulosis, epidermal vacuolization, a band-like lichenoid infiltrate, necrosis of keratinocytes, and marked pigment incontinence (Figures 2 and 3).3
LPP can be diagnosed clinically based on the characteristic lesions, which are dark brown to gray or gray-blue round or oval macules that grow and eventually coalesce. The lesions vary in size, are smooth, and have well-defined borders. Patterns include diffuse, reticular, annular, linear (blaschkoid), and LPPI, as in our patient. Dermoscopic findings include blue-gray and brown-gray dots and globules consistent with the presence of melanophages and pigment incontinence in the dermis. Red lines may be seen, indicating capillary ectasia in the superficial dermis.
Differential Diagnosis
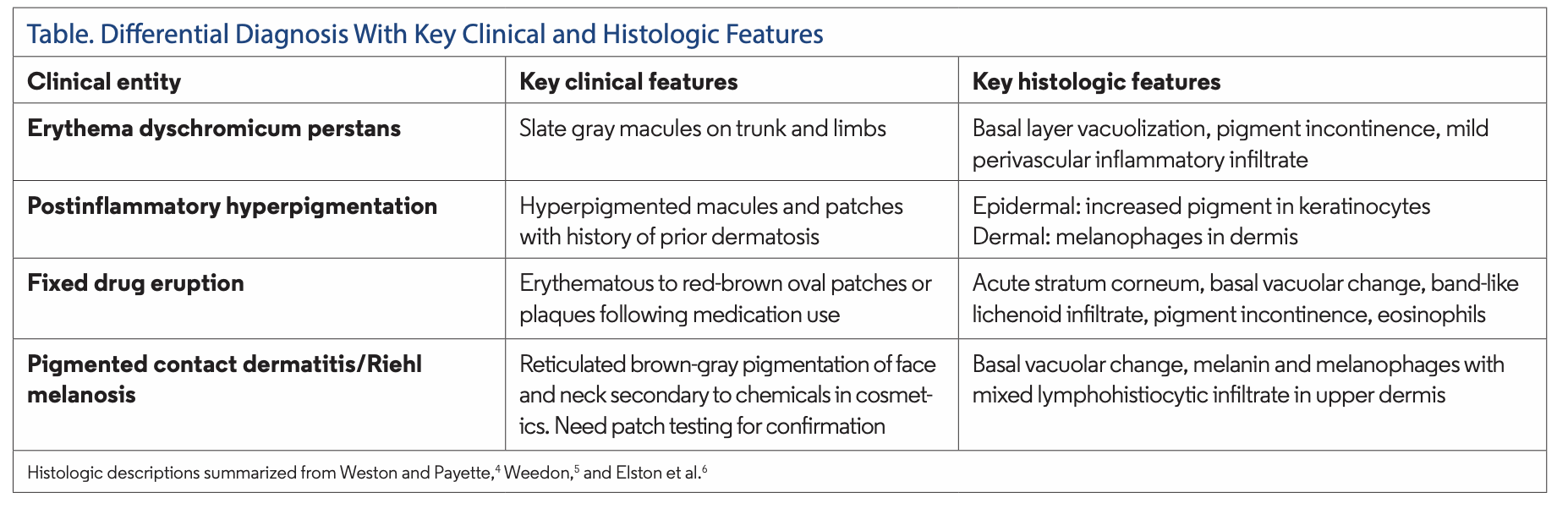
The Table5,6 features the most common differential diagnoses.
Histology
Biopsy from right axilla demonstrated scattered necrotic keratinocytes within the epidermis with a band-like lymphocytic infiltrate in the superficial papillary dermis with melanin incontinence consistent with LPP. The histologic differential is extensive, as it includes numerous entities with a superficial band-like lymphocytic infiltrate, including but not limited to LP, erythema dyschromicum perstans, lichen nitidus, lichen striatus, fixed drug eruption, lichenoid drug eruption, erythema multiforme, LP-like keratotis, etc. See Figures 2 and 3 for photomicrographs.
Pathogenesis
LPP is characterized by a CD8+ T-cell mediated immune response in which an attack of epidermal keratinocytes causes pigment incontinence.2 This initial rapid inflammatory infiltrate is followed by a long noninflammatory regression phase with deposition of melanin in the dermis. As in LP, keratinocytes focally expressing HLA-DR are especially prone to attack.2
Diagnosis and Management
The diagnosis is largely clinical but can be supplemented by histologic examination. Treatment options include medium- to high-potency topical steroids, tacrolimus, hydroquinone, Q-switched laser (1064 nm), oral steroids, topical retinoids, dapsone, and isotretinoin.2 It can be difficult to treat and response rates are variable as all the treatments are based on anecdotal data.
Our Patient
We reached a diagnosis of LPPI via clinicopathologic correlation. Our patient improved dramatically following an intramuscular injection of triamcinolone acetonide and judicious use of a mid-potency topical corticosteroid.
Conclusion
LPPI is an underreported variant of LP. Pathogenesis is driven by CD8+ autoreactive T cells that attack keratinocytes causing a lichenoid inflammatory pattern.2 Correlation of clinical and histopathological information allows the dermatologist to make the diagnosis. Topical and systemic corticosteroids are the most commonly used treatments. Proper diagnosis of this entity is important to allow the physician to select the most appropriate treatment and manage patient expectations of resolution, as it can be difficult to treat.
References
References
1. Pock L, Jelínková L, Drlík L, et al. Lichen planus pigmentosus-inversus. J Eur Acad Dermatol Venereol. 2001;15(5):452-454. doi:10.1046/j.1468-3083.2001.00347.x
2. Robles-Méndez JC, Rizo-Frías P, Herz-Ruelas ME, Pandya AG, Ocampo Candiani J. Lichen planus pigmentosus and its variants: review and update. Int J Dermatol. 2018;57(5):505-514. doi:10.1111/ijd.13806
3. Mohamed M, Korbi M, Hammedi F, et al. Lichen planus pigmentosus inversus: a series of 10 Tunisian patients. Int J Dermatol. 2016;55(10):1088-1091. doi:10.1111/ijd.13295
4. Weston G, Payette M. Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015;1(3):140-149. doi:10.1016/j.ijwd.2015.04.001
5. Weedon D. Weedon's Skin Pathology. 3rd ed. Churchill Livingstone/Elsevier; 2010.
6. Elston DM, Ferringer T, Ko C, Peckham S, High W, DiCaudo, D. Dermatopathology. 3rd ed. Elsevier; 2019.



















