Laser and Energy-Based Device Safety in Skin of Color: A Stepwise Framework
On the first day of Dermatology Week, Dr Vincent Richer, a Vancouver-based dermatologist, offered a practical framework for minimizing post-inflammatory pigment alteration (PIPA), particularly post-inflammatory hyperpigmentation (PIH), in patients with skin of color.
“Laser treatments cannot be used on darker skin, that’s absolutely a myth,” Dr Richer stated. He emphasized that dermatologists, regardless of background, must develop the knowledge and clinical ability to treat patients with skin of color. “We cannot use as a cop-out that we ourselves don’t have skin of color to not have the knowledge and the practical ability to treat our patients.”
His approach begins with assessing the patient’s individual risk. A thorough history of pigmentary response and examination of high-friction areas like the shins or chest can offer insight. Hyperpigmentation in palmar creases may also signal elevated PIH risk.
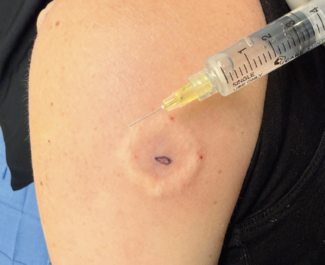
For higher-risk individuals, test spots—targeting a discreet area—are a valuable tool to evaluate response before full treatment.
“We don’t need to be doing test spots all the time,” Dr Richer said, “but they can be helpful in complex or unfamiliar cases.”
Device and wavelength selection is the most critical step. Dr Richer warned against lasers and intense pulsed light systems that directly target melanin, especially short wavelengths. Longer wavelengths, like long-pulsed Nd:YAG lasers, are typically safer as they bypass the melanin-rich basal layer.
For resurfacing, Dr Richer recommended low-density, low-fluence settings and a conservative start. Technologies such as radiofrequency microneedling with insulated needles and microfocused ultrasound were highlighted as safer options due to deeper heat delivery that avoids melanin-rich zones.
“Start slow and go slow,” Dr Richer advised. “We might need more treatments to reach the outcome, but the incremental approach helps reduce complications.”
On pre- and post-treatment prophylaxis, Dr Richer acknowledged that while clinical evidence is limited, some strategies are commonly used. Topical hydroquinone is widely used pre-treatment, especially in high-risk patients, despite limited evidence. Post-treatment photo protection and topical corticosteroids have stronger support for reducing PIH risk. Oral tranexamic acid shows potential, but more research is needed in the context of laser procedures.
He concluded with a reminder not to over-rely on devices when safer alternatives may suffice. For some patients, topical agents, oral therapies, or simply monitoring may provide safer and equally effective results.
His message to colleagues was clear, effective treatment planning for patients with skin of color requires thoughtful risk assessment, careful technique, and respect for melanin—not avoidance, but precision.
For more meeting coverage, visit the Dermatology Week newsroom.
Maximize your experience by adding up to 90 days of on-demand access. Find the package that works for you. Upgrade here.
Reference
Richer V. Cosmetic laser treatment of skin of color. Presented at: Dermatology Week; May 14–16, 2025; Virtual.