Gram-Negative Cellulitis Presenting as Unilateral Lower Extremity Purpura
Chief Medical Editor’s Comment: Sakunchotpanit et al. present an unusual presentation of cellulitis. The clinical picture was very different from how we might expect cellulitis to appear. This case illustrates an important principle of dermatologic diagnosis. Dermatologists are highly adept at identifying different dermatologic conditions based on their characteristic patterns of inflammation. These inflammatory patterns, which are the result of normal immune function, create the distinct clinical pictures that we rely on to make diagnoses. When the immune system is not normal, all bets are offs; an abnormal immune system does not necessarily make normal patterns of inflammation, and any condition may appear in almost any pattern. The patient presented here had chronic kidney disease and a history of leukemia treated with bone marrow transplantation. In this setting, immune function is almost certainly not normal. Impaired immune function not only increased the patient’s susceptibility to unusual infection, but it also led to the infection presenting with atypical findings. When patients have abnormal immune function, it may be valuable to consider the possibility of infection even when skin findings are not suggestive of an infectious process. In the setting of an abnormal immune system, having a low threshold for biopsy may be prudent.
A 54-year-old man with chronic systolic and diastolic heart failure, stage III chronic kidney disease, and B-cell acute lymphoblastic leukemia status post allogenic bone marrow transplantation (with relapse, undergoing blinatumomab salvage therapy) presented with a 1-day history of a painful right lower extremity rash. He denied any preceding trauma to the area, although 2 months prior to presentation he was hospitalized for colonic graft-vs-host-disease (GVHD) complicated by Escherichia coli bacteremia and cytomegalovirus colitis and viremia. He completed a course of cefpodoxime and was continued on ruxolitinib 10 mg twice daily, prednisone 15 mg daily, and prophylactic valganciclovir. On admission, he had neither fever nor leukocytosis. Venous Doppler ultrasonography was negative for deep vein thrombosis. Computed tomography with contrast of the right leg showed mild subcutaneous edema without soft tissue fluid collection. Blood cultures grew 4+ E. coli and he was started on meropenem. Dermatology was consulted for further evaluation of his rash.
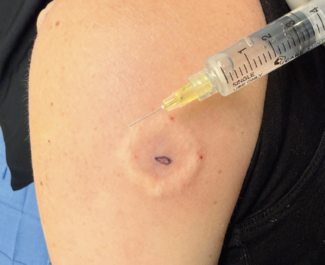
Physical examination revealed scattered purpuric macules coalescing into patches on the right medial leg and ankle, tender and warm to the touch (Figure 1 and Figure 2). There was 2+ pitting edema present on both legs. Skin biopsy revealed superficial to deep perivascular inflammatory infiltrate predominantly composed of neutrophils and extravasated erythrocytes. Tissue culture grew 2+ E. coli, confirming a diagnosis of gram-negative cellulitis, and the patient’s rash ultimately resolved with antibiotics.

Discussion
Cellulitis is an acute infection of the deep dermal and subcutaneous tissue that classically presents as tender, edematous, warm, and expanding unilateral erythema. Most cases of cellulitis are attributed to gram-positive bacteria found on the skin, such as Streptococcus pyogenes and Staphylococcus aureus, but gram-negative organisms have also been implicated in various settings, including E. coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Haemophilus influenza (often facial cellulitis in children), Vibrio vulnificus (associated with saltwater exposure), Eikenella (following human bites), and Pasteurella multocida (following dog or cat bites). While most cases of cellulitis follow bacterial entry via mechanical skin defects, such as tinea pedis, venous stasis disease, or injury, noncutaneous entry of bacteria into the skin from the bloodstream or other infected organs can also occur, particularly in patients with heart failure, cirrhosis, chronic renal failure, immunosuppression, or hematologic malignancy.1-4
Although pathogenic E. coli strains commonly cause urinary tract infections, enteric disease, and meningitis, this microbe can be a rare cause of skin and soft tissue infection.2,3 For our patient, particularly in the setting of immunosuppression and hematologic malignancy, we postulate that mesenteric venous congestion secondary to heart failure and colonic GVHD may have caused increased bowel edema and permeability, predisposing him to E. coli translocation and consequent bacteremia and cellulitis— a mechanism that has been previously described.2

Conclusion
While cases of gram-negative cellulitis can certainly present similarly to classic cases of cellulitis, they can also have unique physical examination findings—presenting with bullae or with purpura as highlighted by our patient. Biopsy for pathology, as well as tissue culture, can help differentiate gram-negative cellulitis from other etiologies of purpura in medically complex patients with multiple comorbidities
Goranit Sakunchotpanit is an M4 at Tufts University School of Medicine, Dr Dufner is the director of digital health and clinical innovation in the department of dermatology at Tufts Medical Center, and Dr Hoot is the director of the Contact Dermatitis Clinic in the department of dermatology at Tufts Medical Center in Boston, MA.
Disclosure: The authors report no relevant financial relationships.
References
1. Raff AB, Kroshinsky D. Cellulitis: a review. JAMA. 2016;316(3):325-337. doi:10.1001/jama.2016.8825
2. Nguyen JK, Hoxhallari E, Daffy J. An unusual case of Escherichia coli cellulitis and bacteremia in an immunocompetent patient. Dermatol Reports. 2023;15(2):9603. doi:10.4081/dr.2023.9603
3. Jabbour JF, Kanj SS. Gram-negative skin and soft tissue infections. Infect Dis Clin North Am. 2021;35(1):157-167. doi:10.1016/j.idc.2020.10.008
4. Horowitz Y, Sperber AD, Almog Y. Gram-negative cellulitis complicating cirrhosis. Mayo Clin Proc. 2004;79(2):247-250. doi:10.4065/79.2.247