Technique to Reduce Wound Size: The Double-Opposing Purse-String and Horizontal Continuous Closure Algorithm
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Surgical reconstruction of complex wounds requires considerable planning to ensure optimal patient outcomes. A conservative approach utilizing the lower tiers of the reconstructive ladder is preferred, especially in patients with comorbidities lending to a higher risk of poor wound healing. A simplified, low-risk solution with a double-opposing purse-string suture (PSS) and horizontal continuous closure technique may be particularly helpful in reducing the need for more complex techniques of wound reconstruction in select patient populations.
Methods. A retrospective chart review was performed on all patients who underwent reconstruction with the double-opposing PSS technique (N = 57) by the senior author (B.J.W.) at the University of Louisville between 2019 and 2022.
Results. A total of 46 patients and 57 wounds underwent the double-opposing PSS and horizontal continuous closure technique as directed by the algorithm. The average defect size before and after was 61 and 12 cm2, respectively. A 2-tailed paired t test analysis was performed to explore the relationship between the pre- and post-closure defect size (P = .0003, t (44) = 3.9, 95% CI). A total of 21 wounds required a skin graft, meaning 63% of the wounds were successfully closed without the use of skin graft as a result of the double-opposing PSS technique. In addition, of those 21 wounds, the skin grafts, as well as the donor site sizes, were smaller.
Conclusions. This approach to wound closure demonstrates usefulness in reducing the size of or need for skin grafts in complex wound patients, particularly in those with comorbidities. The majority of patients underwent successful closure of their complex defects in various areas (eg, face, extremities) with this technique. Residual defects requiring skin graft allowed for a smaller graft and, thereby, donor site. Ultimately, this technique reduces the risk of complex complications by simplifying and reducing wound size.
Introduction
Plastic and reconstructive surgeons assess several factors when determining the most appropriate approach to the reconstructive ladder, including wound characteristics, patient comorbidities, and technical difficulty. Notably, patients who are elderly, have chronically elevated serum glucose, have a history of smoking, are on long-term systemic corticosteroid therapy, have poor nutritional status, and are undergoing chemotherapy or radiation have been shown to experience poor wound healing.1-8 The presence of any one or a combination of these factors adds to the complexity of reconstruction, since a skin graft may be required because of a lack of other viable options on the reconstructive ladder; this technique can help minimize the area of skin graft needed, as well as donor site morbidity. One solution to this is the use of a purse-string suture (PSS) technique, which we revisit in this paper.
PSS techniques were originally described by Cannon and Murray in 1954 in the context of facial injuries.9 Soon after, the technique was used to close cutaneous surgical defects of the breast, urethra, and umbilicus, and were later shown to be effective in the repair of postoperative surgical wounds in the context of skin cancer excision—a particularly useful application.10,11 The PSS technique can provide complete wound closure in the setting of small wounds and, with larger wounds, the PSS technique reduces the need for a significant amount of donor skin for grafting by reducing the wound size.12 In addition, the PSS technique is associated with a fast learning curve and shorter operating times, and provides hemostatic function.13-15 In this study, we aimed to reduce skin graft burden with a double-opposing PSS and horizontal continuous closure algorithm, specifically in a series of 46 cases associated with various anatomical sites and surgical indications.
Methods
A retrospective cohort study was performed through a chart review of 46 patients (57 wounds) who underwent some form of adjacent tissue rearrangement at the University of Louisville Hospitals between 2019 and 2022. This study was reviewed, and a waiver of informed consent was granted by the University of Louisville Institutional Review Board according to 45 CFR 46.101(b) (IRB #23.0739) as it was determined to be secondary research for which informed consent is not required under federal guidelines. Patients with incomplete records with respect to variables examined were excluded. All reconstructions were completed by the senior author (B.J.W.). This algorithm for complex wound closure calls for a double-opposing PSS technique, with a potential need for horizontal continuous closure or split-thickness skin graft (STSG), as depicted in Figure 1. If complete closure of the defect is achieved with double-opposing PSS, then no further action is required (Figure 1, Outcome 1). However, if the defect remains open after the double-opposing PSS, the remaining area to be closed should be measured. If this area is less than 2 cm2, operators should proceed with a horizontal continuous closure (Figure 1, Outcome 2); if this area is 2 cm2 or larger, operators should proceed with an STSG (Figure 1, Outcome 3). The decision to use a full-thickness skin graft (FTSG) vs an STSG was determined on a case-by-case basis depending on the anatomical location and patient characteristics.
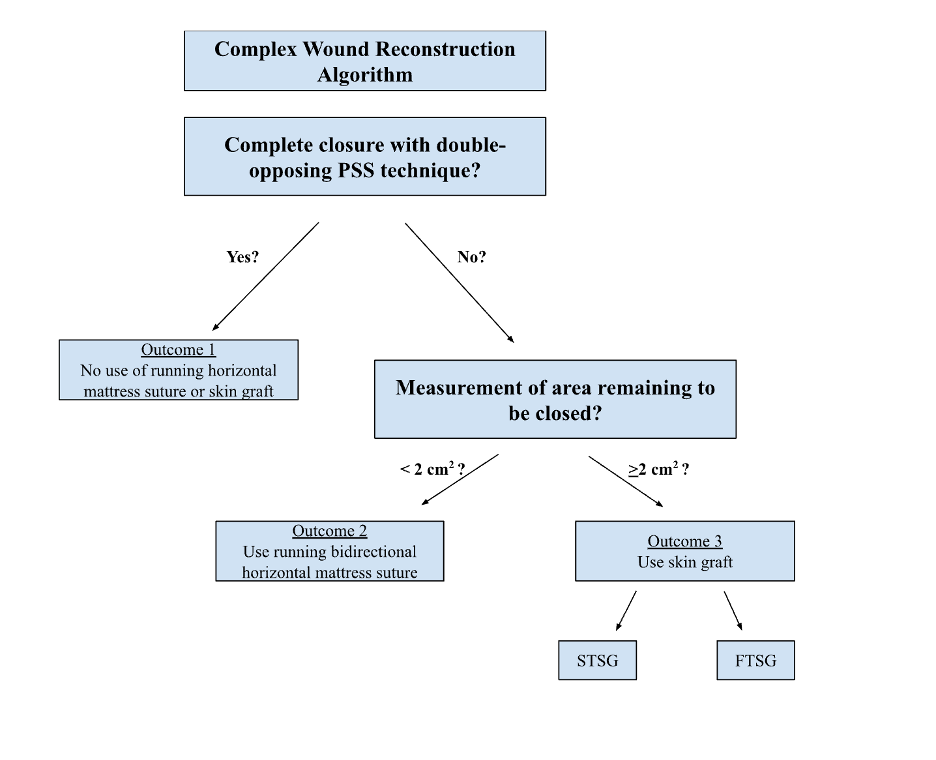
Figure 1. Decision-making flowchart for complex wound reconstruction with PSS and STSG. FTSG = full-thickness skin graft; PSS = purse-string suture; STSG = split-thickness skin graft.
Surgical technique
The double-opposing PSS is performed by running subcuticular sutures in a clockwise fashion around the wound using an absorbable monofilament (often 0 polydioxanone [PDS] or 2-0 PDS) on a circle taper extra-large needle starting at the 12 o’clock position (Figure 2A). Each entry point is placed at a uniform depth in the dermis and travels 3 to 5 millimeters radially from the epidermal edge. Importantly, we recommend intentional travel between bites, as this redistributes any redundant tissue to help close the defect. This technique is repeated around the wound until reaching the first entry point and both ends of the suture are positioned at 12 o’clock. Then, a second stitch is started at the 6 o’clock position and circles counterclockwise until both ends of this suture are positioned at 6 o’clock (Figure 2B). The ends of this second stitch are then drawn taut, tied down, and buried (Figure 2C), followed by the ends of the first stitch in the same fashion. Of note, the first and last bites for both stitches are deep to ensure that the knots can be buried when tying.
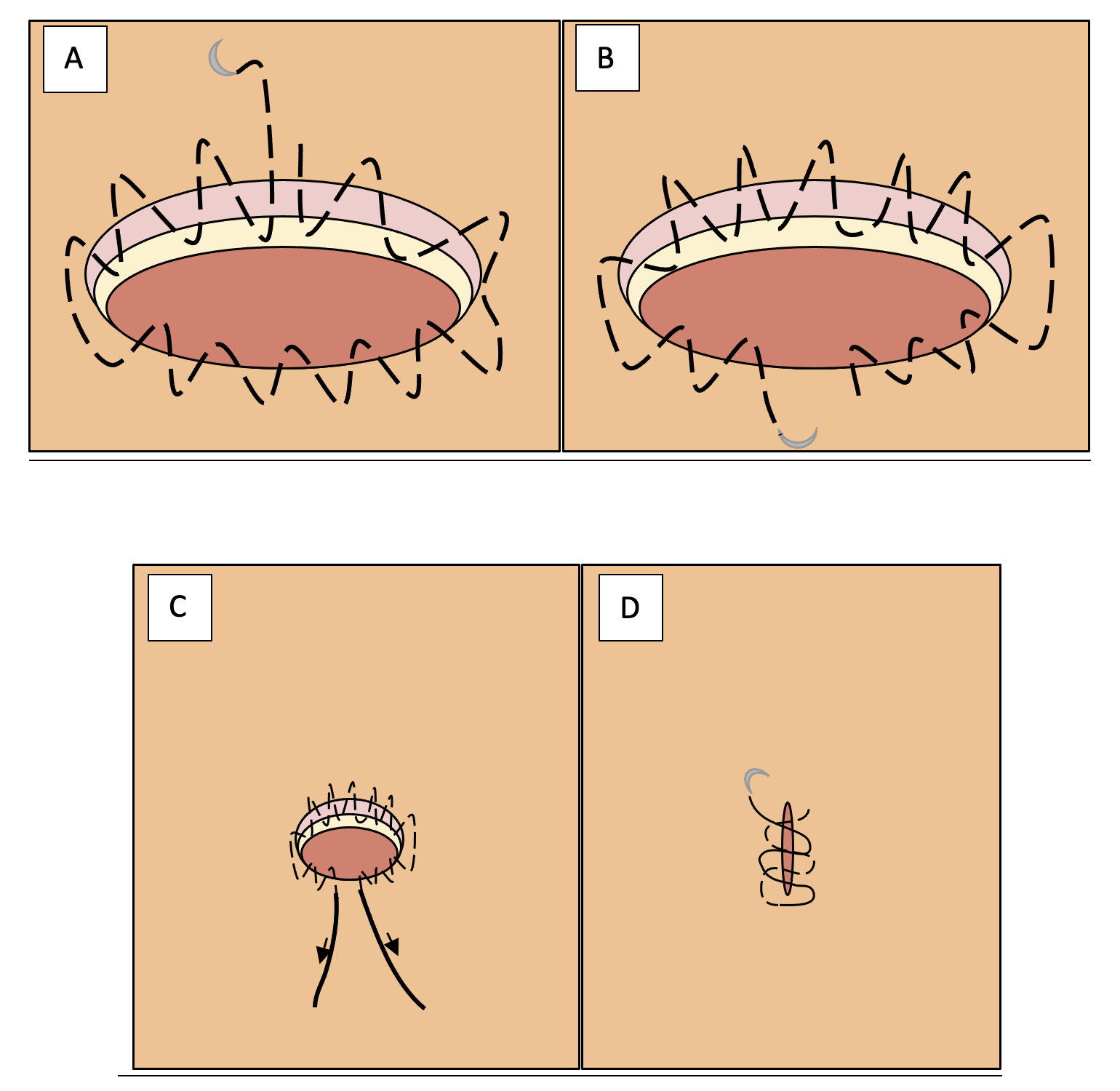
Figure 2. Cartoon depiction of the double-opposing purse-string suture with bidirectional running horizontal mattress suture. (A) First PSS entering the dermal-epidermal junction at the 12 o’clock position, running in a clockwise direction staying within the dermis, and exiting the dermis again at the 12 o’clock position. (B) Second PSS entering the dermal-epidermal junction at the 6 o’clock position, running in a counterclockwise direction staying within the dermis, and exiting the dermis again at the 6 o’clock position. (C) Fastening both ends of both sutures and burying the knots. (D) Running bidirectional horizontal mattress. PSS = purse-string suture.
If the wound does not achieve complete closure with double-opposing PSS and is less than 2 cm2, a running bidirectional horizontal mattress closure is conducted using 3-0, 4-0, or 5-0 PDS and/or 3-0 polypropylene (Prolene) (Figure 2D). If the defect size is 2 cm2 or larger after the double-opposing PSS, a skin graft is indicated to achieve complete wound closure (Figure 1, Outcome 3). If an STSG is indicated, a graft is harvested with a dermatome between 0.014 and 0.018 inches thick and meshed to an appropriate ratio. If an FTSG is indicated, a graft is harvested using the standard excision technique and subsequently defatted. The graft is fashioned to the defect and secured with a 3-0 or 4-0 chromic gut suture. The recipient site is dressed with a non-adherent dressing, then bolstered or covered with a wound vacuum-assisted closure device to provide compression and optimize graft take. The donor site is dressed with an occlusive dressing and wrapped as necessary. Splints are generally used for grafted extremities.
Results
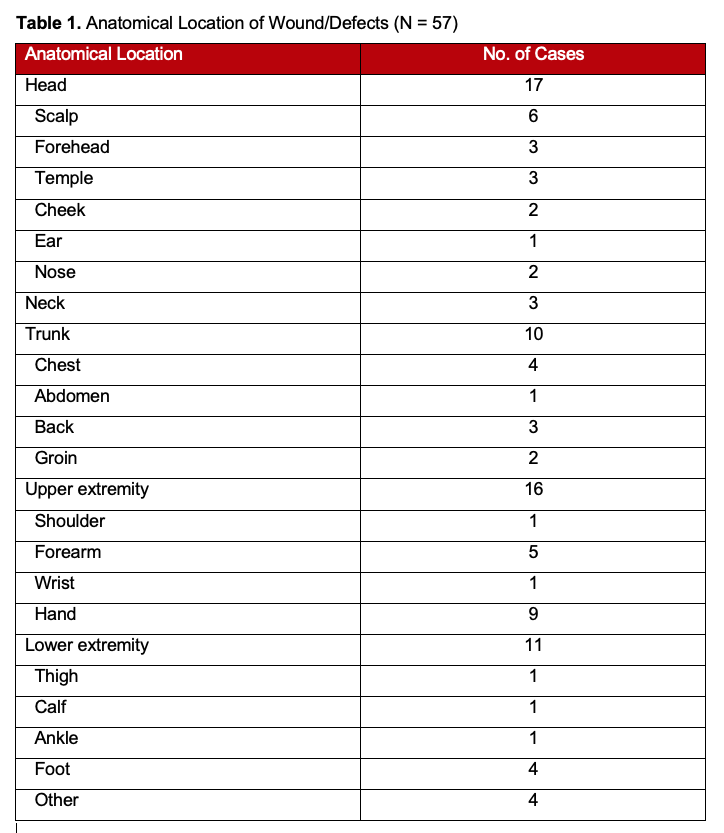
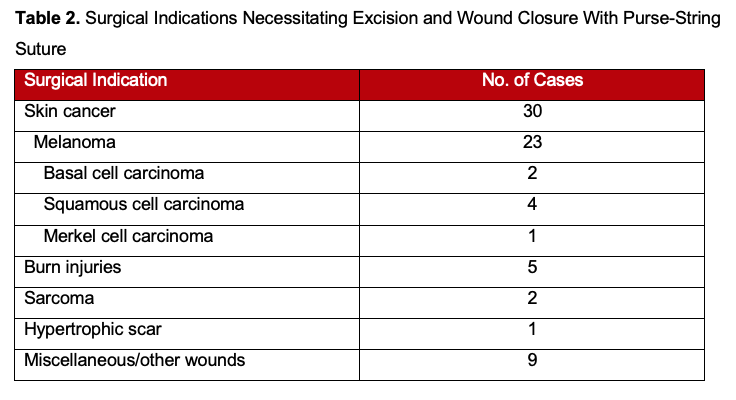
Retrospective review of medical records from 46 patients who underwent the double-opposing PSS showed the average age of patients to be 61 years (range, 24-94 years). Many defects were located on the head, upper extremity, or lower extremity, as shown in Table 1. The majority of patients underwent reconstruction and closure with the double-opposing PSS method following skin cancer resection; however, other etiologies included burns, sarcomas, and 1 hypertrophic scar (Table 2). One patient presented with 2 types of skin cancer: melanoma and basal cell carcinoma.
Overall, a total of 46 patients (57 wounds) underwent the double-opposing PSS technique. Of those 46 patients, 9 patients presented with 2 defects and 1 patient presented with 3 defects. The average defect size prior to the technique was 61 cm2. The average defect size after the technique was 12 cm2, an 80% reduction. A 2-tailed paired t test analysis was conducted to explore the relationship between the defect size before and after the double-opposing PSS technique (P = .0003, t (44) = 3.9, 95% CI). Additionally, 21 out of 57 wounds required a skin graft; 17 wounds received an STSG ranging from 0.014 to 0.018 inches. Four wounds received FTSGs, meaning that primary closure was successful in 63% of the wounds, avoiding skin grafting entirely.
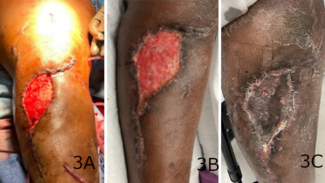
Several cases were of particular interest and are detailed as follows. Figure 3 depicts the case of a 63-year-old female who presented with invasive ductal carcinoma of the left breast. The patient underwent partial mastectomy and radiation therapy. She subsequently developed a cutaneous angiosarcoma of the left breast. Staging scan showed no evidence of metastatic disease, and she underwent completion mastectomy and wide local excision (WLE) of all radiated tissue (Figure 3A). Afterwards, a large defect that was present on her lateral chest wall was circumferentially closed via the double-opposing PSS (Figure 3B) and ultimately a smaller STSG (Figure 3C). STSG was chosen to monitor for recurrence as a more reliable form of surveillance.
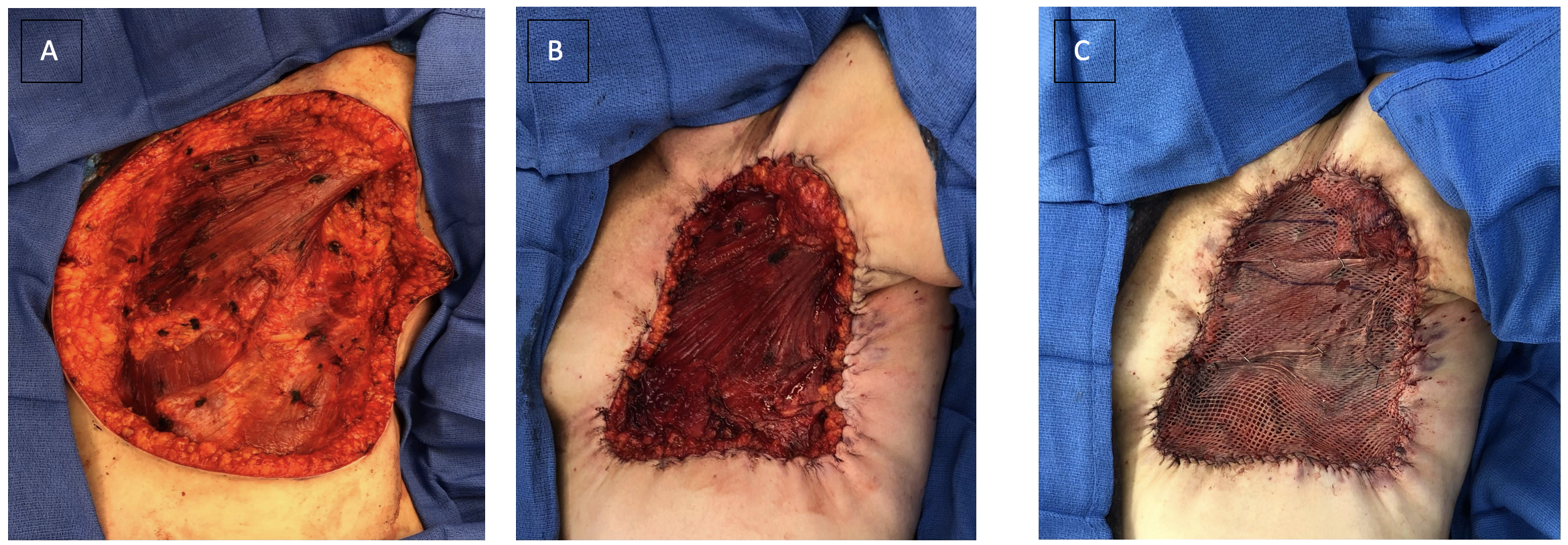
Figure 3. Patient who developed cutaneous angiosarcoma of the left breast following partial mastectomy and radiation therapy for invasive ductal carcinoma. (A) Large defect located on lateral chest wall prior to application of the PSS. Shoulder at the superior aspect of wound and pectoralis major visible superomedially. (B) Defect after double-opposing PSS. (C) Defect after meshed STSG. PSS = purse-string suture; STSG = split-thickness skin graft.
Figure 4 represents the case of a 61-year-old female who presented with stage T1a melanoma on the right ankle. The patient successfully underwent WLE of the melanoma and complete closure with the double-opposing PSS. Figures 5 through 7 are additional cases of melanomas on the upper or lower extremities, which were also treated with WLE. While Figures 5 and 6 were closed primarily with the use of the double-opposing PSS, the patient shown in Figure 6 had a skin graft applied because the tightness of the surrounding skin did not allow for primary closure. As of the writing of this study, there have not been any local recurrences that have required surgical intervention or the need for further biopsies.
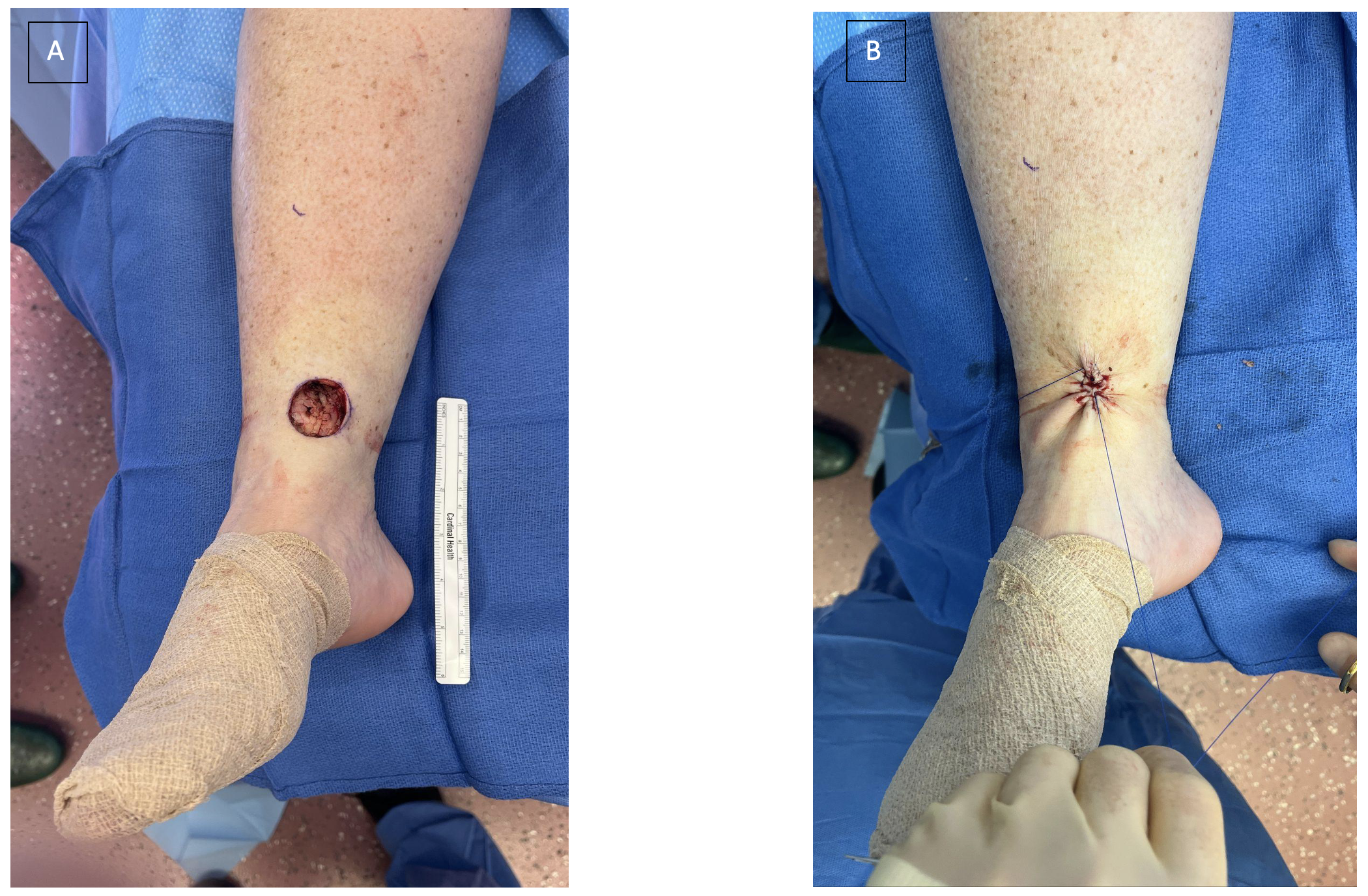
Figure 4. Patient who presented with a T1a melanoma of the right ankle who underwent wide local excision. (A) A defect located on the right ankle prior to application of PSS. (B) Complete closure of right ankle wound using double-opposing PSS. PSS = purse-string suture.
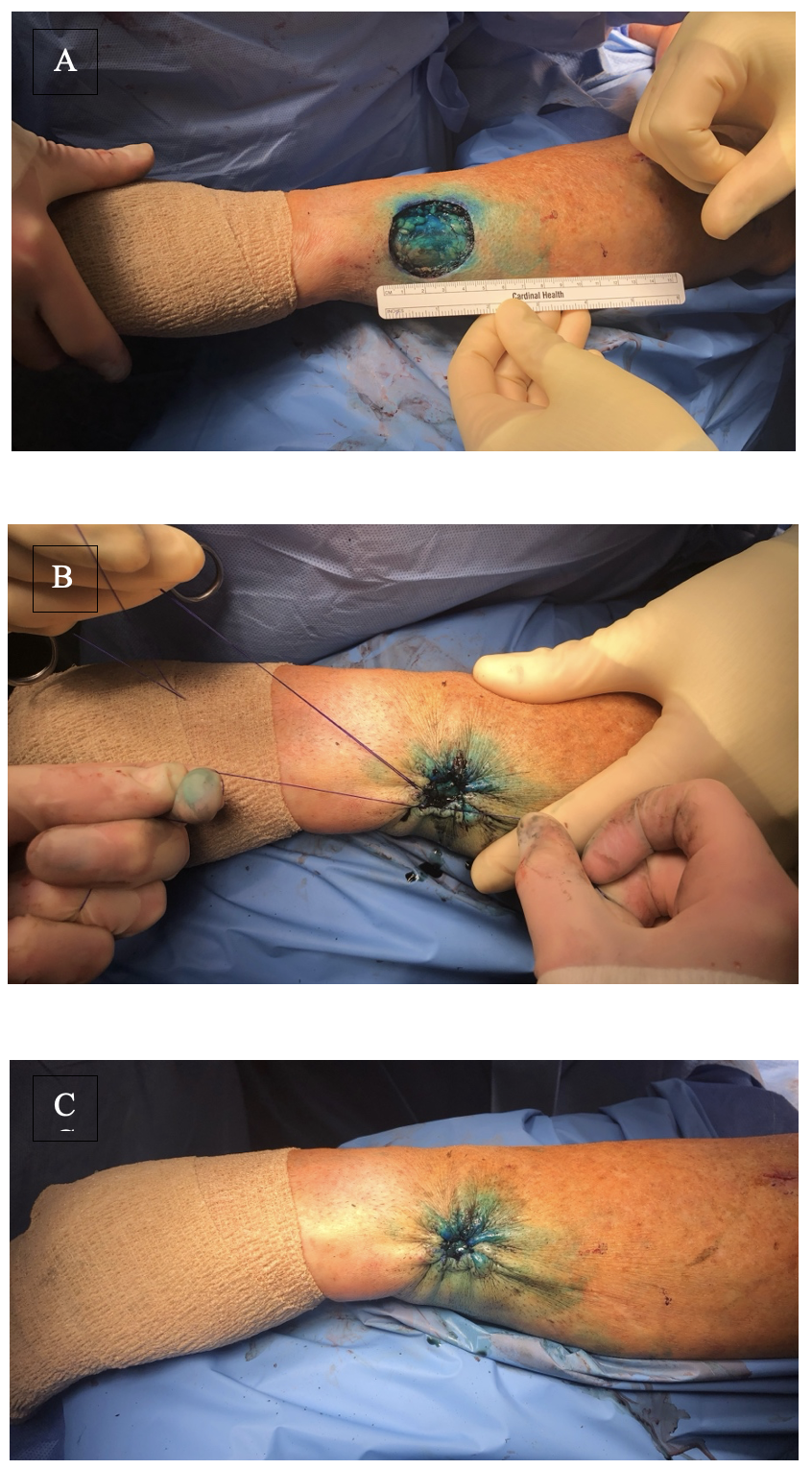
Figure 5. Patient who presented with a T1b melanoma of left forearm who underwent wide local excision. (A) A 5 x 5-cm defect on the dorsal aspect of the left forearm just proximal to the ulnar styloid. (B) Application of second PSS in opposite direction. (C) Complete closure of left forearm defect using the double-opposing PSS without need for a skin graft. PSS = purse-string suture.
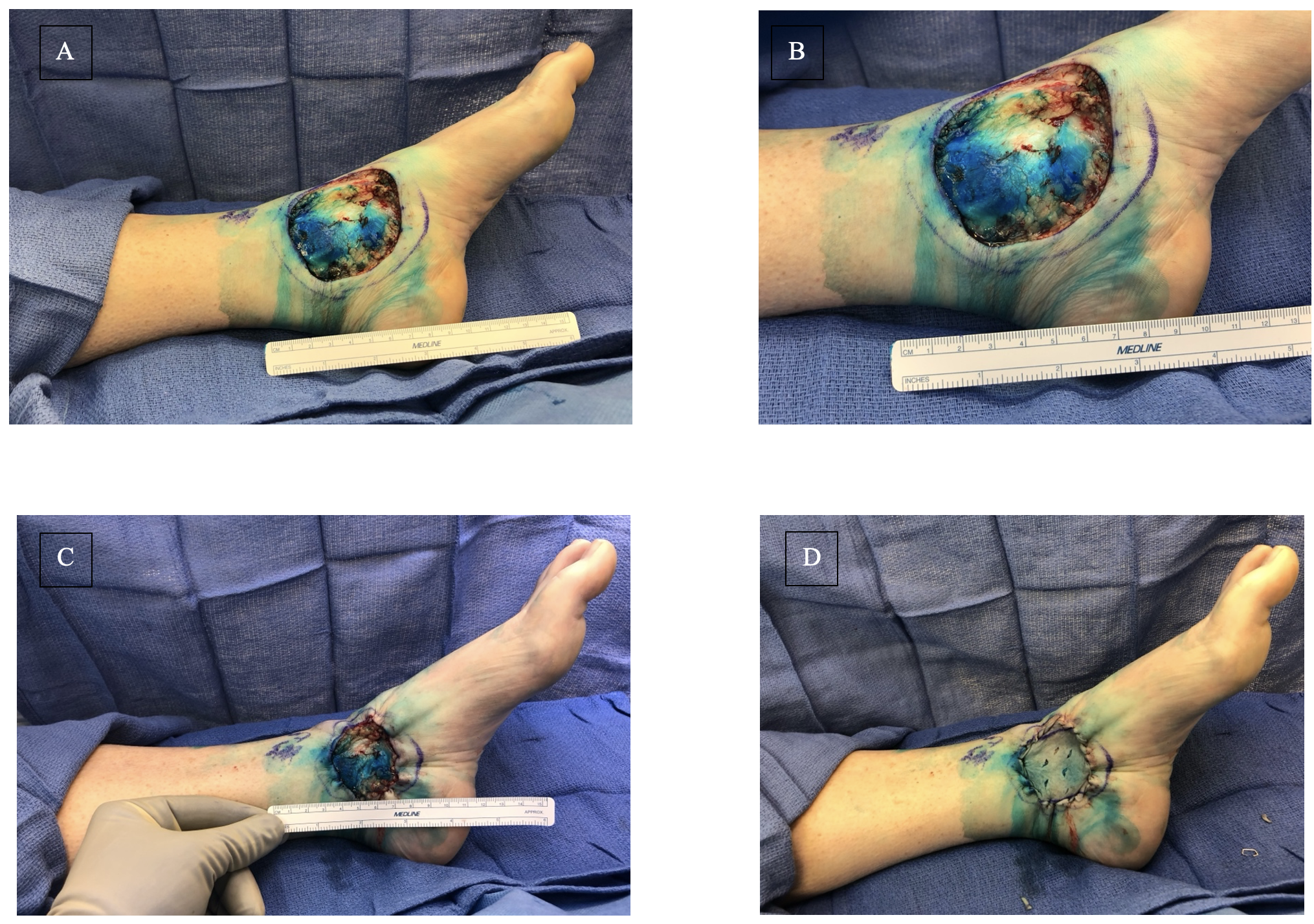
Figure 6. Patient who presented with a T4 nodular melanoma of the left ankle who underwent wide local excision. (A) A 6 x 7-cm defect of the left medial malleolus measuring an overall area of 36 cm2. (B) Close-up image of the defect. (C) Defect measuring 16 cm2 in total area after utilization of double opposing PSS. (D) Application of the split-thickness skin graft from the right thigh and secured with 3-0 chromic sutures. PSS = purse-string suture.

Figure 7. Patient who presented with 0.9-cm thick melanoma of the left ankle and underwent wide local excision. (A) 3-cm defect of the left anteromedial ankle. (B) Complete closure of the left ankle defect utilizing the double opposing PSS without need for a skin graft. PSS = purse-string suture.
Discussion
Since its inception, the PSS has been modified in regard to technique, suture material, and length of time to suture removal, along with implementation of wound undermining and subsequent skin grafting.10,12,16-25 In this study, we utilized the modified double-opposing PSS: a technique that differs from the original procedure in that it has 2 separate purse-string sutures in the dermal-epidermal subcuticular plane that are superimposed upon one another. In the double-opposing PSS, 1 suture travels clockwise and the other counterclockwise, with one beginning at the 12 o’clock position and the other at 6 o’clock. The second purse-string suture allows for additional incorporation of the surrounding tissue for wound closure, reducing the size of the defect beyond what is possible using the original technique and possibly allowing for total closure of the wound.19 In another description of the PSS technique, the suture is threaded along the circumference of the wound, never passing over the defect itself. The needle passes through the epidermis approximately 2 to 4 millimeters from the edge, travels 5 to 10 millimeters along the circumference through the dermis and adipose tissue, then returns to the surface and repeats the sequence next to the preceding entrance site.10,12,17 Once the suture has traveled along the entire circumference, the suture is pulled taut and subsequently knotted, completing the technique.17
The double-opposing PSS is a simple, fast, and low-cost reconstructive technique that results in smaller wound size and thereby less donor skin necessary for grafting, or, in many cases, the complete closure of complex wounds.12,26 Therefore, this is a favorable option for patients who experience poor wound healing and for whom it is important to minimize donor site morbidity from skin graft harvest and locoregional flaps are not a good option.8 In addition, the PSS technique can preserve wound margins and orientation in such a way that oncologic tissue post-excision can be referred to using a clock-face template;27 if residual cancer is identified at the 3 o’clock location, it will remain at 3 o’clock following the PSS, whereas the use of other techniques such as locoregional flaps may distort the tissue and make reexcision more difficult should margins be positive.13,27 If reexcision is required, the suture can be removed to reform the final defect and observe the wound margins more clearly.11 For example, in 1 case study, the first PSS reduced the defect by 59%, which was further reduced to 8% of its original size by the second suture.
Furthermore, the double-opposing PSS generates circumferential distribution of forces, creating small, radiating skin folds that disappear with time, rather than 2 large dog ears that would develop if sutured longitudinally.28 Dog ears can be aesthetically unappealing and have been reported to cause pain and discomfort.29 In our opinion, the avoidance of large dog ears can reduce these complaints. Therefore, the double-opposing PSS is helpful for wounds that are too large for closure using a single PSS and would be best closed circumferentially, as depicted in Figure 3A. It is important to note that the PSS can result in skin-edge ischemia leading to skin necrosis if the PSS is placed too tightly.28 None of our patients reported this complication.
Our algorithm provides standardized recommendations to help guide surgical decision-making in the closure of complex wounds. Large wounds are slow to heal independently and may complicate or delay other adjuvant therapies if allowed to heal by secondary intention alone.30 The algorithm reflects this reality, recommending skin grafts for wounds that remain 2 cm2 or larger following the use of the double-opposing PSS. In wounds that are smaller than 2 cm2 after the double-opposing PSS, horizontal mattress sutures are indicated, as the remaining defects are too small to be closed in this manner.
Our primary goal was to minimize the complications of wound reconstruction in vulnerable patients who are not strong candidates for skin grafts. However, we also helped to improve cosmesis by avoiding a skin graft, which can leave an incongruent tone and irregular texture of the grafted area.10 Most (63%) of our patients achieved successful primary closure of their wounds, avoiding skin grafting entirely. Furthermore, in patients who still required grafting after the double-opposing PSS, the area requiring coverage was reduced by 80%.
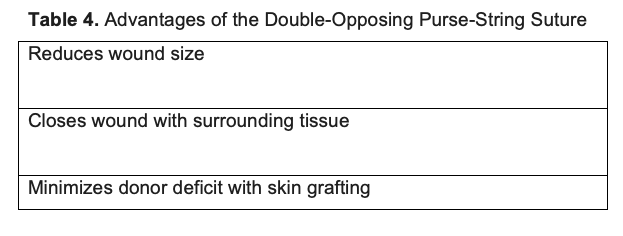
Our cohort presented with a mix of anatomical locations, with most defects located on the head, followed by the upper and lower extremities. Additionally, a number of patients presented with lesions on the neck, chest, abdomen, back, and groin, which were successfully closed with the PSS technique. Most of our patients presented with various skin cancers, though several other surgical indications (eg, wounds secondary to breast reconstruction or knee arthroplasty, nodular lesions, and nasal defects) were included in our study, as described in Table 2. Our results highlight the advantages of the double-opposing PSS (Table 4) and speak to the versatility of this technique, demonstrating that it can be widely employed in numerous anatomical locations to close defects caused by various pathologies.
Limitations
The potential limitations of our study include the relatively small sample size, lack of comparison to a control group, and lack of long-term follow-up, compromising our ability to assess late complications and cosmesis. Additionally, the results were not stratified by age. PSS is noted to be generally more efficacious in the elderly because of the increased skin laxity at advanced ages.28 Though our study included patients between 24 and 94 years old, the average age was 61 years. Further review would be necessary to determine the extent to which patient age impacted our results. However, given that elderly patients are known to experience poor wound healing1–yet they are often quality candidates for PSS–our research underscores the positive impact that avoiding a skin graft via PSS can have on this demographic.
Conclusions
This algorithm provides standardized recommendations for the closure of complex wounds that can aid in surgical decision-making. The use of a double-opposing PSS with an additional horizontal running mattress suture, as directed by the algorithm, allowed most of our patients to avoid skin grafting and reduced the amount of donor skin required for grafting in the remaining patients. The double-opposing PSS is a straightforward reconstructive technique that is helpful in patients with comorbidities who would benefit from conservative wound management.
Acknowledgments
Authors: Alexander L. Mostovych, MS1; Lexina R. Patel, BS1; Kartik Garg, MD2; Quinton L. Carr, BA1; Mitchell Peake, MD3; Ryan Cantrell, BS1; Bradon J. Wilhelmi, MD3
Affiliations: 1University of Louisville School of Medicine, Louisville, Kentucky; 2NYU Grossman School of Medicine, Department of Surgery, New York, New York; 3Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Louisville, Louisville, Kentucky
Correspondence: Bradon J. Wilhelmi, MD, Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Louisville, 550 South Jackson Street, ACB 2nd Floor, Louisville, KY 40202, USA. E-mail: bradon.wilhelmi@louisville.edu
Ethics: The patients in this document have been provided informed consent on the use of their images and granted the use of their images for scientific publications. IRB: University of Louisville IRB - Study# 17.0522
Disclosures: The authors disclose no financial or nonficancial conflicts of interest.
References
1. Coskunfirat OK, Chen HC, Spanio S, Tang YB. The safety of microvascular free tissue transfer in the elderly population. Plast Reconstr Surg. Mar 2005;115(3):771-5. doi:10.1097/01.prs.0000152424.91250.a5
2. Janis JE, Harrison B. Wound healing: part I. Basic science. Plast Reconstr Surg. Feb 2014;133(2):199e-207e. doi:10.1097/01.prs.0000437224.02985.f9
3. Siana JE, Rex S, Gottrup F. The effect of cigarette smoking on wound healing. Scand J Plast Reconstr Surg Hand Surg. 1989;23(3):207-9. doi:10.3109/02844318909075119
4. Anstead GM. Steroids, retinoids, and wound healing. Adv Wound Care. Oct 1998;11(6):277-85.
5. Ruberg RL. Role of nutrition in wound healing. Surg Clin North Am. Aug 1984;64(4):705-14. doi:10.1016/s0039-6109(16)43386-4
6. de Waard JW, de Man BM, Wobbes T, van der Linden CJ, Hendriks T. Inhibition of fibroblast collagen synthesis and proliferation by levamisole and 5-fluorouracil. Eur J Cancer. Jan 1998;34(1):162-7. doi:10.1016/s0959-8049(97)00352-3
7. Wang Q, Dickson GR, Abram WP, Carr KE. Electron irradiation slows down wound repair in rat skin: a morphological investigation. Br J Dermatol. May 1994;130(5):551-60. doi:10.1111/j.1365-2133.1994.tb13098.x
8. Buchanan PJ, Kung TA, Cederna PS. Evidence-Based Medicine: Wound Closure. Plast Reconstr Surg. Sep 2016;138(3 Suppl):257s-270s. doi:10.1097/prs.0000000000002775
9. Cannon B, Murray JE. Plastic surgery: facial injuries. N Engl J Med. Jan 7 1954;250(1):17-23. doi:10.1056/nejm195401072500104
10. Cohen PR, Martinelli PT, Schulze KE, Nelson BR. The purse‐string suture revisited: a useful technique for the closure of cutaneous surgical wounds. International Journal of Dermatology. 2007;46(4):341-247. doi:10.1111/j.1365-4632.2007.03204.x
11. Harrington AC, Montemarano A, Welch M, Farley M. Variations of the pursestring suture in skin cancer reconstruction. Dermatol Surg. Apr 1999;25(4):277-81. doi:10.1046/j.1524-4725.1999.08150.x
12. McCue J, Kalliainen LK. Use of a Purse-String Suture to Reduce Skin Graft Requirements. Ann Surg Oncol. Feb 2018;25(2):471-474. doi:10.1245/s10434-017-6215-6
13. Fioramonti P, Sorvillo V, Maruccia M, et al. New application of purse string suture in skin cancer surgery. International Wound Journal. 2018;15(6):893-899. doi:10.1111/iwj.12941
14. Cammarata E, Zavattaro E, Astolfi S, et al. Purse-string suture versus full-thickness skin graft: An efficacy and safety comparison study. Dermatol Ther. May 2021;34(3):e14909. doi:10.1111/dth.14909
15. Hagen R, Shah N, Yousaf A, Ghareeb E, Zinn Z. Pre-emptive purse-string suture: A novel technique to minimize bleeding risk. J Am Acad Dermatol. Mar 2020;82(3):e85-e86. doi:10.1016/j.jaad.2019.10.030
16. Ciatti S, Greenbaum SS. Modified purse-string closure for reconstruction of moderate/large surgical defects of the face. Dermatol Surg. Mar 1999;25(3):215-9; discussion 219-20. doi:10.1046/j.1524-4725.1999.08155.x
17. Cohen PR, Martinelli PT, Schulze KE, Nelson BR. The cuticular purse string suture: a modified purse string suture for the partial closure of round postoperative wounds. Int J Dermatol. Jul 2007;46(7):746-53. doi:10.1111/j.1365-4632.2007.03253.x
18. Yuen JC. Versatility of the subcuticular purse-string suture in wound closure. Plast Reconstr Surg. Dec 1996;98(7):1302-5. doi:10.1097/00006534-199612000-00032
19. Davis JC, Baillis B, Love WE. Novel stacked double purse-string closure. Dermatol Surg. Dec 2014;40(12):1409-12. doi:10.1097/dss.0000000000000219
20. Cruz AP, Campbell RM, Perlis CS, Dufresne RG, Jr. Double purse-string closure for scalp and extremity wounds. Dermatol Surg. Mar 2007;33(3):369-73. doi:10.1111/j.1524-4725.2007.33076.x
21. Lin H, Li W. Complete closure using a double purse-string closure for skin defects. Dermatol Surg. Sep 2009;35(9):1406-9. doi:10.1111/j.1524-4725.2009.01248.x
22. Marquart JD, Lawrence N. The purse-string lockdown. Dermatol Surg. May 2009;35(5):853-5. doi:10.1111/j.1524-4725.2009.01143.x
23. Nicholas L, Bingham J, Marquart J. Percutaneous buried modification of the purse-string closure. Dermatol Surg. Sep 2014;40(9):1052-4. doi:10.1097/01.DSS.0000452638.60199.d1
24. Patel KK, Telfer MR, Southee R. A “round block” purse-string suture in facial reconstruction after operations for skin cancer surgery. British Journal of Oral and Maxillofacial Surgery. 2003/06/01/ 2003;41(3):151-156. doi:https://doi.org/10.1016/S0266-4356(03)00047-0
25. Peled IJ, Zagher U, Wexler MR. Purse-string suture for reduction and closure of skin defects. Ann Plast Surg. May 1985;14(5):465-9. doi:10.1097/00000637-198505000-00012
26. Simman R, Bach K, Achauer SM. Purse-String Suture Technique in Reducing Surgical Defect Size. Eplasty. 2022;22:ic14.
27. Sezgin B, Kapucu I, Yenidunya G, et al. A practical method for accurate coordination between the plastic surgeon and the pathologist: The clockwork technique. Arch Plast Surg. Jan 2018;45(1):96-97. doi:10.5999/aps.2017.00283
28. Park H, Lee Y, Yeo H, Park H. Surgical refinement of the purse-string suture for skin and soft tissue defects of the head and neck. Arch Craniofac Surg. Aug 2021;22(4):183-192. doi:10.7181/acfs.2021.00297
29. Kang AS, Kang KS. A Systematic Review of Cutaneous Dog Ear Deformity: A Management Algorithm. Plast Reconstr Surg Glob Open. Sep 2020;8(9):e3102. doi:10.1097/gox.0000000000003102
30. Beldon P. Skin grafts 1: theory, procedure and management of graft sites in the community. Br J Community Nurs. Jun 2003;8(6 Suppl):S8, S10-12, S14 passim. doi:10.12968/bjcn.2003.8.Sup2.11552