Congenital Upper Extremity Anomalies Misdiagnosed as Ulnar Longitudinal Deficiency
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Patients with a congenital hand plate or upper limb anomaly, a dysplastic ulna, or a syndrome may present with morphologic forms commonly misdiagnosed as ulnar longitudinal deficiency (ULD).
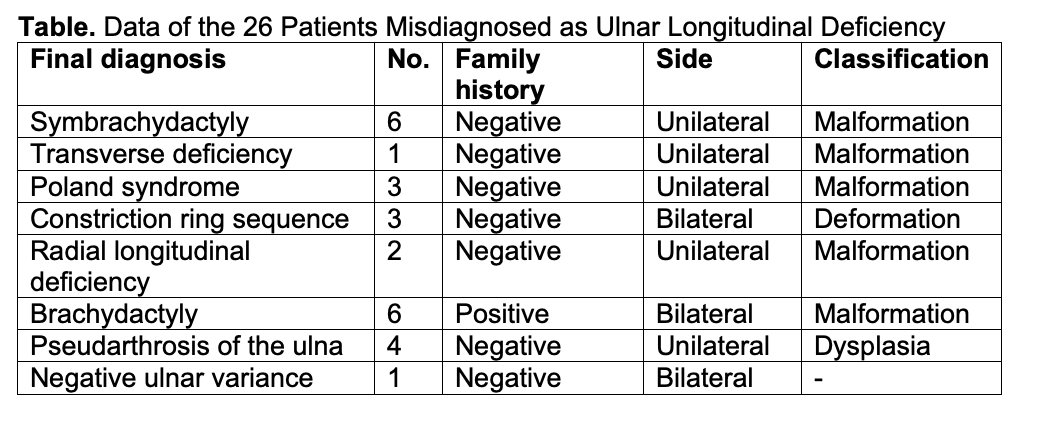
Methods. Patients who had been misdiagnosed with ULD over the past 35 years were identified from the hospital database. Twenty-six patients with photographs and/or conventional radiographs that could be adequately reproduced were enrolled in the study.
Results. In 16 unilateral cases, the final diagnosis changed to symbrachydactyly (6 cases), Poland syndrome (3 cases), transverse deficiency (1 case), radial longitudinal deficiency (2 cases), and congenital pseudarthrosis of the ulna with osteolysis in patients with neurofibromatosis type 1 (4 cases). In 10 bilateral cases, the final diagnosis changed to constriction ring sequence (3 cases), brachydactyly (6 cases), and congenital bilateral negative ulnar variance in a patient with central metacarpal medullary stenosis. This research presents the findings of the 7 most illustrative cases and focuses on their differential diagnosis. Additionally, the literature review summarizes the most common congenital anomalies included in the differential diagnosis of ULD, presenting their clinical and/or radiographic features as detected in patients referred to our service.
Conclusions. A detailed evaluation of patients with even simple unilateral congenital hand or upper limb anomalies is invaluable to the diagnostic investigation. The treating pediatrician, clinician, or surgeon should also be sufficiently familiar with the clinical and radiographic features of congenital anomalies and the long list of syndrome-related deficiencies that the differential diagnostic process of ULD includes. Missed or misinterpreted findings in patients with congenital hand or upper limb anomalies, usually recorded after single diagnosis documentation, may result in a misdiagnosis of ULD and delayed detection of associated congenital, medical, or syndromal disorders.
Introduction
Ulnar (postaxial) longitudinal (ray) deficiency (ULD), also referred to as ulnar clubhand or dysmelia, includes a spectrum of congenital abnormalities affecting the ulnar border of the hand or upper limb with a broad phenotypic variability and severity. It mostly appears as a sporadic, commonly unilateral anomaly that may be associated with other musculoskeletal, though usually not systemic, anomalies. Initial studies classified ULD as hypoplasia of the ulna, partial absence, and total absence (hemimelia). Various classification systems have since been published, including all potential anomalies of the hand, the upper extremity, and associated medical or musculoskeletal abnormalities and syndromes.1,2 The anomalies of the ulna detected in ULD do not include bowing or deformation.3
This research presents 26 patients who were misdiagnosed with ULD, with the aim to indicate the wide variety of congenital anomalies considered in the differential diagnosis of ULD, assess the value of the clinical and radiographic findings, and define specific features that may help yield a definite diagnosis. It also presents a literature review of other congenital upper limb anomalies considered in the differential diagnostic investigation of ULD, including illustrative cases from a large population referred to our service.
Methods and Materials
This study retrospectively reviewed patients who were referred to our orthopedic department with a misdiagnosis of ULD over the past 35 years. The available notes on the history and physical examination, the clinical photographs, and the plain radiographs were examined; patients with photographs and/or conventional radiographs that could not be adequately reproduced were excluded. Twenty-six patients (15 males and 11 females, 24 children and 2 adults) were enrolled in the study. All patients were referred with single-diagnosis documentation. The screening at our service included musculoskeletal abnormalities of the other limbs and trunk and potential medical or syndromal disorders. Computed tomography, magnetic resonance imaging, and investigational genetic techniques, including DNA testing for neurofibromatosis, were not performed.
In this study, the terms ulnar deficiency, hypoplasia, or dysplasia were used to describe abnormalities of the ulnar aspect of the forearm or hand, while deficiency, hypoplasia, or dysplasia of the ulna pertained only to abnormalities of the ulna itself. Hypoplasia of the ulna indicated an undersized—in length, width, or both—straight ulna. Deficiency of the ulna indicated hypoplasia, partial defect of an ulnar remnant, undersized or not, or complete absence. Finally, dysplasia indicated the radiographic appearance of curving angulation, bowing, tapering, thickening, or an abnormal congenital bone configuration other than an undersized straight bone involving the whole or a portion of the ulna.
Results
The anomalies were unilateral in 16 cases and bilateral in 10 cases. The final diagnosis in the 16 unilateral cases changed to symbrachydactyly (6 cases), Poland syndrome (3 cases), transverse deficiency (1 case), radial longitudinal deficiency (2 cases), and congenital pseudarthrosis of the ulna with osteolysis in patients with neurofibromatosis type 1 (NF1) (4 cases). In the 10 bilateral cases, the diagnosis changed to constriction ring sequence (3 cases), brachydactyly (6 cases), and congenital bilateral negative ulnar variance associated with asymptomatic ulnar impingement syndrome in a patient with central metacarpal medullary stenosis (1 case). The anomalies presented as sporadic limb deficiencies with no family history in 20 cases and positive family history in the 6 patients with brachydactyly. In the 4 patients with congenital pseudarthrosis of the ulna, a positive family history of NF1 was evident. This study used the updated Oberg-Manske-Tonkin (OMT) classification of congenital hand and upper limb anomalies.4 In the 16 unilateral cases, there were 12 malformations and 4 dysplasias (tumorous conditions); the anomalies involved the hand plate in the 6 cases with symbrachydactyly and the upper limb in the other 10 patients. In the 10 bilateral cases, there were 3 deformations and 6 malformations of the hand plate; however, the negative ulnar variance could not be classified. The patients’ data are briefly presented in the Table.
The 7 most illustrative cases with a final diagnosis of symbrachydactyly, Poland syndrome, transverse deficiency, radial longitudinal deficiency, brachydactyly, congenital pseudarthrosis of the ulna, and congenital bilateral negative ulnar variance, respectively, are reported below in detail.
Case 1
The first patient was a 30-month-old boy with a left-hand anomaly characterized by 4 shorter and smaller ulnar fingers than the contralateral hand, syndactyly between the index and middle finger, and normal thumb anatomy. Hypoplasia involving the phalanges of the 4 ulnar digits was diagnosed on the radiographs. He was referred with a diagnosis of ulnar deficient hand.
Physical examination at our service showed 4 hypoplastic but functioning ulnar digits, incomplete cutaneous (simple) second web syndactyly, and relatively normal thumb anatomy. He had symmetric movement of the shoulders, elbows, and forearms. No other abnormalities of the upper limb and chest wall were evident.
The radiographs further diagnosed brachymesophalangism and mild hypoplasia of the proximal and distal phalanges of the 4 ulnar digits. There was no hypoplasia of the 4 ulnar metacarpals, but their ossification nuclei were smaller than those of the contralateral hand. Mild hypoplasia of the proximal phalanx of the left thumb was also diagnosed. No abnormality was evident in the ossification nuclei of the carpal and forearm bones. The pediatric evaluation revealed no associated medical or syndromal disorders. The final diagnosis was the short-finger type of symbrachydactyly (Figure 1).

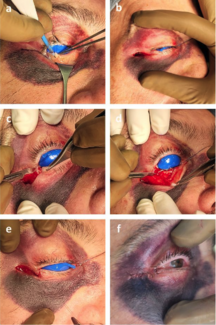
Figure 1. A 30-month-old boy with left short-finger type of symbrachydactyly.
Case 2
The second patient was a 21-year-old man with a left-hand anomaly characterized by loss of the distal phalanx and nail of the fifth finger, hypoplasia of the 4 ulnar fingers, and normal thumb anatomy. Hypoplasia of the middle phalanges of the central fingers, with the severity of shortening increasing from the index to the ring finger, and hypoplasia of the terminal and proximal phalanges of the 4 ulnar fingers had been diagnosed on the radiographs. He was referred with a diagnosis of ulnar deficient hand.
Physical examination at our service showed a smaller left upper limb and hand compared with the right side, with 4 ulnar digits that were shortened but functioning. The syndactylies of the second, third, and fourth web spaces had been surgically released when he was 4 years old. There was a narrowing of the first web and a single palmar crease. He had symmetric movement of the shoulders, elbows, and forearms.
The radiographs showed a single interphalangeal joint of the fifth finger and mild hypoplasia of the metacarpals. The skeletal appearance of the thumb, wrist, and distal forearm bones appeared normal. The chest wall and shoulders were also clinically examined. There were no apparent chest wall abnormalities, but a very mild elevation of the left scapula, indicative of Sprengel’s deformity, and mild thoracic scoliosis were evident. The final diagnosis was Poland syndrome (Figure 2).
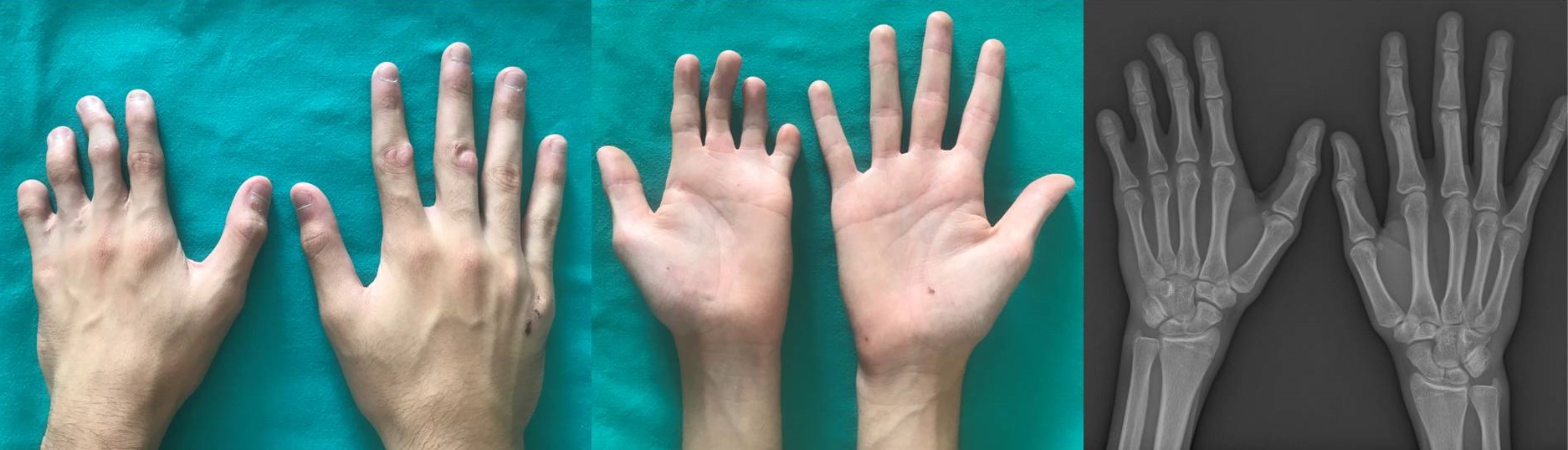
Figure 2. A 21-year-old man with Poland syndrome and unilateral hand anomalies. There is first web hypoplasia and a single palmar crease. Syndactyly release of the second to fourth web spaces is also evident. The radiograph shows a shortening of the central middle phalanges and a single interphalangeal joint of the fifth finger.
Case 3
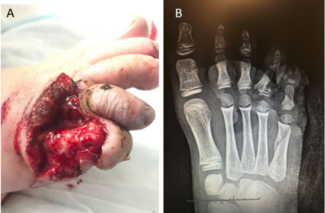
The third patient was an 8-year-old boy with congenital amputation through the left wrist and limited ipsilateral elbow flexion-extension and forearm rotation. Dislocation of the radiohumeral joint, negative ulnar variance, and bowing of the ulna were diagnosed on the radiographs of the affected upper limb; both ossification centers of the ulna were present. He was referred with a diagnosis of ULD with wrist amputation.
Physical examination at our service showed a shortened left upper extremity without soft tissue nubbins, and it focused on the differential diagnosis of the 2 deep skin folds of the distal stump. The level of the deficiency was at the distal end of the radius, the forearm segment was considered complete, and there was no evidence of carpal ossification. Dysplasia of both forearm bones proximal to the level of deficiency was diagnosed on the radiographs. The latter was determined by the curving angulation of the radius and bowing of the ulna. The final diagnosis was forearm transverse deficiency without ectodermal elements (Figure 3).

Figure 3. An 8-year-old boy with unilateral forearm transverse deficiency and skin invaginations at the distal part of the deficient limb. The radiograph shows dysplasia of the forearm bones proximal to the level of the deficiency and congenital dislocation of the radial head.
Case 4
The fourth patient was a 13-year-old girl with a 4-fingered left hand characterized by a mildly abducted and shortened fifth finger ray and thumb aplasia. There was bilateral reduced elbow flexion-extension and forearm rotation. Bilateral radiohumeral dislocation, partial absence of the fifth left metacarpal, and aplasia of the left thumb and first metacarpal were diagnosed on the radiographs. She was referred with a diagnosis of ULD with complete thumb absence.
Physical examination of the left hand at our service showed no hypoplasia of the fifth finger, 4 functioning digits, and a stable wrist. Partial fusion of the fourth and fifth metacarpal, resulting in a “Y” shaped, proximally branched, hypertrophied ulnar metacarpal and hypoplastic distal part of the fifth metacarpal articulating with the proximal phalanx of the fifth finger, was evident on the radiographs. In addition, aplasia of the trapezium, scaphoid hypoplasia, potential bilateral lunotriquetral coalition, and normal appearance of the phalanges of the 4 fingers and distal forearm bones were also evident. The pediatric evaluation revealed no associated medical or syndromal disorders. The final diagnosis was left radial longitudinal deficiency (Figure 4).

Figure 4. A 13-year-old girl with radial longitudinal deficiency. The hypertrophic proximal part of the ulnar metacarpal suggests congenital partial fusion between the fourth and fifth metacarpal.
Case 5
The fifth patient was a 12-year-old boy who presented with bilateral hand anomalies characterized by shortening of the left fourth and fifth fingers and the right fourth finger. Shortening of the left fourth and fifth metacarpal, the right fourth metacarpal, and partial fusion of the epiphyses of the involved metacarpals were diagnosed on the radiographs. He was referred with a diagnosis of a bilateral ulnar deficient hand.
Physical examination at our service showed that the shortened hand rays were functioning, and there was also bilateral shortening of the fourth and fifth toes. The patient was short in stature without mental, facial, or dental abnormalities. There was a positive family history with a male-to-male transmission. All involved members of the family had brachydactyly and were short in stature with no other congenital anomalies or genetic conditions.
The radiographs further diagnosed a broadening of the shortened metacarpals, short middle phalanges of the fifth fingers, and short distal phalanges of the thumb. The fourth and fifth metatarsals were short and broad on both sides. The pediatric evaluation revealed no systemic anomalies or associated medical or syndromal disorders. The final diagnosis was isolated brachydactyly type E (Figure 5).
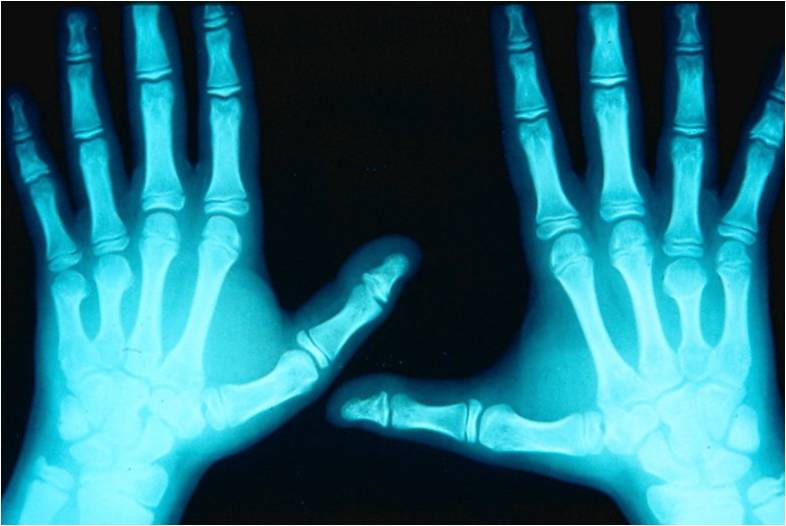
Figure 5. A 12-year-old boy with isolated asymmetric bilateral brachymetacarpia.
Case 6
The sixth patient was a 9-year-old boy with shortening and bowing of the right forearm manifested at birth. There was a positive family history of NF1 in his mother, and the patient was also diagnosed with NF1. Congenital pseudarthrosis of the ulna with a dysplastic appearance and an absent distal ulnar diaphysis, radial and ulnar bowing, and radiohumeral dislocation were diagnosed on the radiographs of the affected upper limb. The patient had been treated conservatively. He was referred with a diagnosis of neglected ULD in a patient suffering from NF1.
Physical examination at our service showed no forearm tenderness, a stable wrist with no deficiencies of the wrist and hand, limited ipsilateral elbow flexion-extension and forearm rotation, scoliosis, and hyperpigmented lesions on his body consistent with café au lait macules of underlying NF1.
The radiographic follow-up evaluation showed pseudarthrosis of the ulna at its middle third and a tapering end of the proximal third, while the distal third presented as a thin intermittent sclerotic line with a residual distal meta/diaphysis and epiphysis. Marked bowing of the radius with proximal migration of the dislocated radial head was also evident. The final diagnosis was isolated congenital bowing-pseudarthrosis of the ulna with resorption of the middle diaphyseal third due to osteolysis in a patient with NF1 (Figure 6).
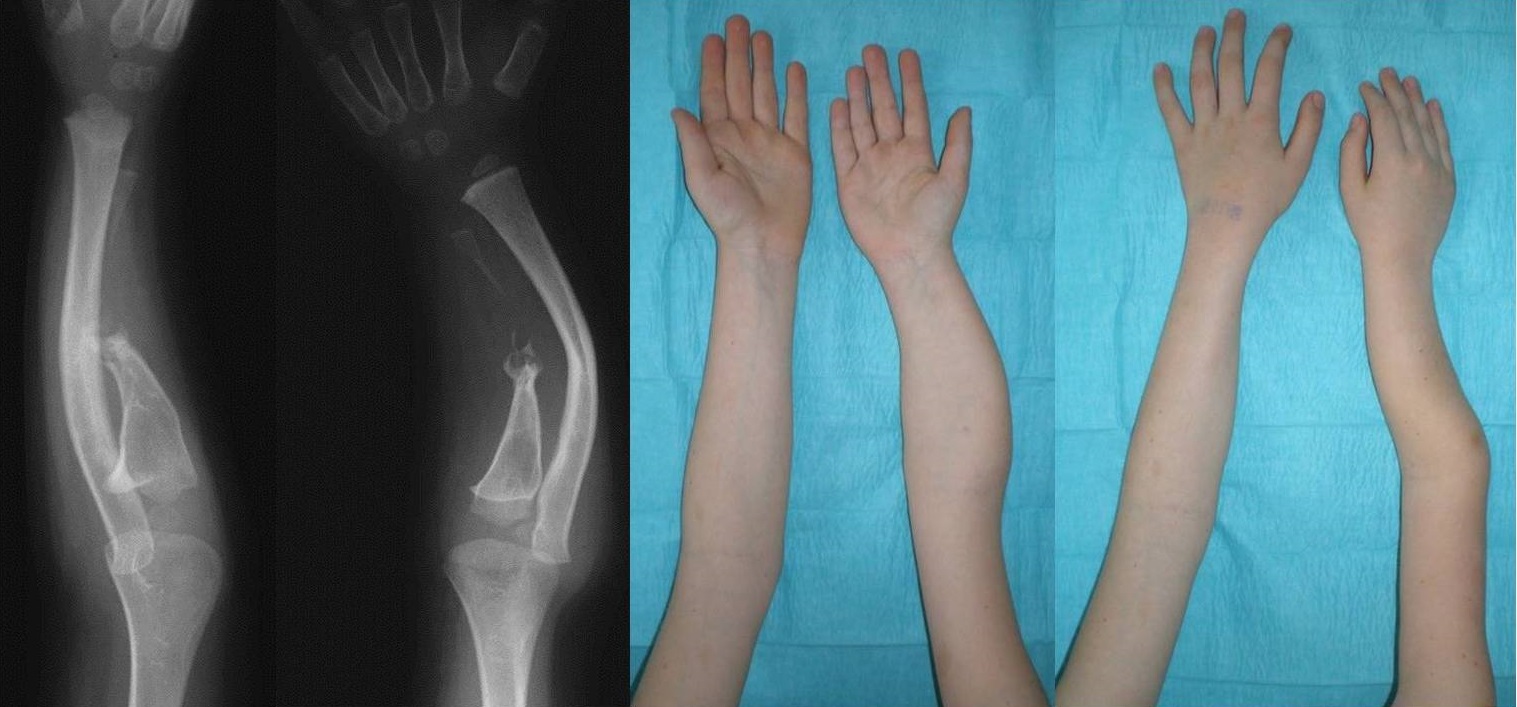
Figure 6. Congenital angulation-pseudarthrosis of the ulna with osteolysis in a boy with neurofibromatosis type 1. The radiographs were taken when the boy was 3 years old and the photographs when he was 9 years old.
Case 7
The seventh patient was a 30-year-old woman who presented with right wrist pain after a sports injury. There was no evidence of a fracture line on the radiographs. She had a full recovery after a 3-week protection. The radiographic follow-up evaluation indicated potential negative ulnar variance; a radiograph of both wrists was requested, which showed bilateral scalloping of the distal radius caused by a shortened ulna impinging on the distal radius proximal to the sigmoid notch. A bilateral metacarpal hypoplasia was additionally diagnosed on the radiographs involving the second to fourth metacarpals. She was referred with a diagnosis of bilateral ULD.
Physical and systemic examination, laboratory studies, and tests for autoimmune diseases at our service showed no abnormal findings. There was no radiographic evidence of similar changes in the metatarsals and no evidence of dwarfism or other syndromal disorders in the patient and her family. The radiographic appearance of obliteration of the central metacarpal intramedullary spaces was considered a variant. The final diagnosis was congenital bilateral negative ulnar variance associated with asymptomatic ulnar impingement syndrome (Figure 7).

Figure 7. A 30-year-old woman with bilateral negative ulnar variance associated with asymptomatic ulnar impingement syndrome. Diminished bilateral medullary cavity width is evident in the second to fourth metacarpals.
Literature review
Congenital upper limb anomalies may be due to nongenetic, molecular, and genetic causes. Congenital hand anomalies with bilateral involvement usually have a genetic basis. Nongenetic cases usually occur sporadically, with 1 hand involved and the feet not affected. They may be due to external factors such as amniotic bands and rings, vascular disruptions, or teratogens. However, most are due to a single mutated gene with low penetrance or may be polygenic as a result of several mutated genes.5
The differential diagnosis of the various phenotypic manifestations of congenital hand and upper limb anomalies may be difficult, even for pediatric hand experts. A multidisciplinary team assessment of experienced hand surgeons, utilizing clinical images and radiographs in a consensus-seeking diagnostic investigation, is most significant to yield a definite diagnosis, especially in patients with atypical or overlapping features.6-8 In addition, all patients with a hand or upper limb anomaly should always be examined for potential syndromes.9
The anomalies detected in ULD may occasionally be confused with other congenital anomalies of the hand and upper limb or with various syndromes. The literature suggests that the differential diagnosis of ULD should include symbrachydactyly with its overlapping malformations and associated syndromes, constriction ring sequence, and Apert syndrome. Overlapping malformations of symbrachydactyly include transverse deficiency, central deficiency, hypodactyly, and brachydactyly; symbrachydactyly may also appear with Poland, Möbius, Klippel-Feil, Turner, Sprengel, and DiGeorge syndromes.10-12 Syndrome-related ulnar anomalies may occur with orofacial malformations and various syndromal disorders, most commonly Cornelia de Lange, femur-fibula-ulna, and ulnar-mammary syndromes.5,13
The clinical and radiographic findings are usually sufficient to classify hands with fewer than 5 skeletal digits.14 Oligodactyly with a normal or hypoplastic thumb and normal or near-normal forearm bones may be a type of ULD. However, it can also be a central deficiency type or a combined type of ULD with either central or radial longitudinal deficiency.15 Various authors have detected a high incidence of thumb and first web (radial-sided) deficiencies in patients with ULD; however, that failed to reproduce in teratogenic drug-induced experimental studies. Although this association suggests postulating 2 separate insults in its pathogenesis, it is more likely that a single insult is responsible.16
The most common hand and upper limb anomalies included in the differential diagnosis of ULD are described below.
Symbrachydactyly-transverse deficiency
Symbrachydactyly is mostly a sporadic unilateral anomaly, predominantly involving the left hand, presenting with shortened or absent central digits with relative sparing of the border ones, eventually forming an atypical cleft hand.12,17 Even to expert hand surgeons, it remains an obscure clinical entity.18 It is also undefined whether it is a discrete and separate hand anomaly.19 Its classification includes the mild phenotype of 2 or 3 short fingers or toes, hypoplasia of the middle phalanges, as well as variable syndactyly of the affected digits20 and the oligodactylic (atypical cleft hand), monodactylic, and peromelic (resembling transverse amputation at the metacarpophalangeal joint level) anomalies (Figure 8).21,22 The reduction begins in the middle phalanges and proceeds proximally. The distal phalanges may also be hypoplastic, but a part of them is always present. The anomaly may typically progress to the ulnar digit and then the thumb. The relationship between symbrachydactyly and terminal transverse deficiency has been investigated, concluding that transverse deficiency through the forearm represents a proximal continuum of symbrachydactyly. Both abnormalities may typically present with a shortened upper extremity, skin invaginations, and digital nubbins with rudimentary nails, although the latter may be missing in transverse defects. The radiographic appearance of bone dysplasia proximal to the deficiency is fundamental in the definitive diagnosis of transverse deficiency.11,23
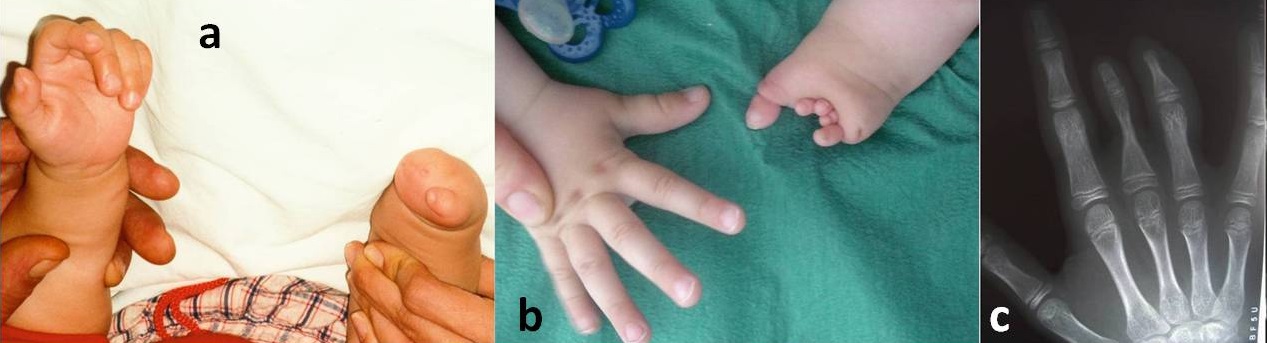
Figure 8. Symbrachydactyly (with ectodermal elements) involving the hand plate. (A) The monodactylic type presents with a thumb and four associated digital remnants. (B) The oligodactylic type (atypical cleft hand or central digit hypoplasia) presents with thumb and fifth digit hypoplasia and nubbins with terminal ectodermal elements for fingers 2, 3, and 4. (C) The short-finger type is evident in a 14-year-old boy with a sporadic unilateral shortening of the third and fourth finger with no functional impairment and no other upper limb or chest wall abnormalities. The third ray seems to be the primary involvement with an ulnar and proximal proceeding of the reduction. The index finger is not affected. There is a single interphalangeal joint in the third and fourth fingers, indicating a missing middle phalanx, while the distal phalanx of the third finger is hypoplastic. There is no shortening of the proximal phalanx of the third finger, but its distal and middle portions are hypoplastic.
Other authors reported a 7-type classification of symbrachydactyly incorporating transverse deficiency24 and evaluated function according to hand morphology25 and the appropriate surgical management regarding the status of the border digits and the clinical or radiographic features.26 Symbrachydactyly refers to a failure of axis formation and differentiation of the hand plate or the entire upper limb (Poland or excluding Poland syndrome) and, similarly, transverse deficiency in the OMT classification of congenital hand malformations.18 The inconsistency of combining terminal transverse defects, in which the ectodermal elements are missing, with symbrachydactyly, in which the initial deficiency is upper-extremity mesodermal underdevelopment (hypoplasia of the middle phalanges) with preservation of ectodermal fingertip elements (fingernails, nail beds, and distal phalangeal tufts),27 has been addressed in the updated OMT classification. In the latter, symbrachydactyly with ectodermal elements and transverse deficiency without ectodermal elements define malformations involving either the entire upper limb due to abnormal axis formation (either Poland syndrome or whole limb excluding Poland syndrome) or the hand plate due to abnormal axis differentiation.4 Although the description of the level of deficiency and the presence of ectodermal elements are valuable in differentiating between symbrachydactyly and transverse deficiency, the former has been considered a more significant determining factor for diagnosis.28 The recent term “central digit hypoplasia” refers to the phenotype of thumb and fifth finger hypoplasia with nubbins of soft tissue at the level of the metacarpophalangeal joint of fingers 2, 3, and 4.29
Poland syndrome
Poland syndrome is usually a sporadic unilateral anomaly that may present with a variable phenotypic spectrum involving the hand, upper limb and shoulder, chest cage, spine, breast and nipples, and soft tissues. It includes all disturbances of pectoral development, with or without ipsilateral symbrachydactyly. Poland syndrome is a potential diagnosis for all patients suffering from a unilateral atypical cleft hand. The syndrome is often underdiagnosed and underreported because the majority of patients are asymptomatic or have few functional manifestations.30,31 The theory of subclavian artery disruption during the sixth week of gestation is the most prevailing one regarding pathogenesis.10 Various reports have mentioned that hand deformity may not be present or substantial in all patients. The range of the radiographic abnormalities of the middle phalanges may include hypoplasia or aplasia, a central nidus, a rounded or truncated appearance, and cone-shaped epiphyses. They have also indicated that chest asymmetry may become evident at puberty, and proposed a classification of the wide range of hand and upper limb anomalies.32-35 Poland syndrome is commonly associated with syndactyly, like Apert syndrome, and pediatricians should be aware of this potential association to avoid a missed diagnosis in children with cutaneous syndactyly.36
Constriction ring sequence
Constriction ring sequence (amniotic band disruption sequence or amniotic constriction band syndrome) is usually a sporadic anomaly with no generally accepted pathogenesis. It is the priority entity in the differential diagnostic process from the amputation preceded by symbrachydactyly or transverse deficiency. It involves the central finger rays more than the thumb and may present with circumferential or incomplete hand constrictions, lymphedema, acrosyndactyly, and amputation. It usually involves 3 extremities, with greater involvement of the upper extremity, especially the distal aspects, and the short digits lack rudimentary fingers and nails. Careful evaluation for potential associated anomalies should always follow its diagnosis.37-39 It appears like a traumatic amputation with no proximal bone hypodysplasia on the radiographs (Figure 9).17,21,40,41 Constriction ring sequence defines a deformation congenital hand anomaly in the OMT9 and its updated classification.4

Figure 9. Constriction ring sequence. (Top row) Annular constrictions, right thumb and left index lymphoedema, and bilateral amputations of the digits are evident in a 3-year-old boy. The radiograph shows no bone hypoplasia proximally to the amputated fingers and the typical tapering. (Bottom row) Transverse types of the amputated stumps and acrosyndacyly of the central finger rays are evident in 2 other patients. The radiographs show no bone hypoplasia proximally to the amputated fingers and the typical tapering.
Hypodactyly
Hypodactyly is a nonhereditary unilateral transverse deficiency, distinct from symbrachydactyly or constriction ring sequence. It is not associated with syndromes or potential causative diagnoses. Distal phalanges are absent, followed sequentially by the middle and proximal phalanges. Unlike symbrachydactyly, ectodermal elements are missing, and bony deficiencies progress from the distal phalanges proximally and from the 2 ulnar digits to the long and index fingers and finally to the thumb, which is the least affected digit. The involved digits are fleshy and broad, and the metacarpals are not involved.11
Cleft hand
Cleft hand may present with considerable phenotypic variability of bone and soft tissue suppression in the central elements, typically bilateral. Inheritance is autosomal dominant with incomplete penetrance, but it may also occur spontaneously. Clinical presentation may include minor shortening to absence of the third ray with a cleft; aplasia of 2, 3, or 4 radial rays with no cleft; syndactyly between the thumb and index finger; and cleft feet or facial clefts. The definition of the typical cleft hand aims to avoid confusion with the atypical cleft hand that is characteristic of symbrachydactyly: the cleft hand shape has a ‘V’ configuration, unlike the ‘U’ in symbrachydactyly. Most hands with an even, considerably malformed appearance have satisfactory function.42 Cleft hand may occur as an isolated trait or alongside other disorders such as camptodactyly and clinodactyly, with or without delta phalanges. Fusion or duplication of rays and transverse (cross) bones may also be evident.
Despite the reported differences, the confusion with symbrachydactyly remains (Figure 10).43,44 Unlike with symbrachydactyly, the reduction proceeds radially, with only the fifth finger remaining in the monodactylic type, which renders the definition of symbrachydactyly as a type of cleft hand—even atypical—inconsistent; furthermore, in the cleft hand, there is no hypoplasia or dysplasia of the proximal bones.27 Cleft hand defines an abnormal proximal-distal axis (late limb patterning/differentiation) malformation of the hand plate in the updated OMT classification.4 Split hand/foot malformation is the recent definition according to genetic terms. The term “cleft hand complex” indicates the complicated combinations of cleft hand with central polydactyly and osseous syndactyly.45-47

Figure 10. Cleft hand (split hand/foot malformation). (A) The radiograph shows a bilateral central cleft with asymmetrical malformations, including fusion and duplication of rays, and the transverse or cross bone specific to cleft hand on the right hand. (B) A 13-year-old girl with a sporadic malformation involving cleft hands and feet; no orofacial or musculoskeletal anomalies and medical conditions were evident.
Thumb hypoplasia- radial longitudinal deficiency
Thumb hypoplasia may appear in a range of forms, from a slightly reduced thumb size with no associated thenar abnormalities to thumb aplasia with complete loss of all thumb structures and radial carpal bones. It may exist either independently or in the context of radial longitudinal deficiency.48,49 Aplasia of the thumb with proximal synostosis of the fourth and fifth metacarpal is evident in chromosomal aberrations of the 13q region.50
Radial longitudinal deficiency may be inherited in the autosomal recessive or dominant forms, although most cases are due to spontaneous mutations. It is commonly associated with bone and soft tissue anomalies and syndromes.51 It may present with a large spectrum of preaxial abnormalities mainly involving the radius, the radiohumeral joint, the radial side of the wrist, and the thumb, as well as with 2 types of synostosis (radioulnar and fourth-fifth metacarpal), which are relatively common.52,53 Radial longitudinal deficiency and hypoplastic thumb define malformations involving the hand plate due to abnormal radioulnar (anteroposterior) axis differentiation.4
Brachydactyly
Brachydactyly presents with phalangeal, metacarpal, and/or metatarsal shortening or absence and may occur as an isolated trait or in combination with other anomalies. In isolated, non-syndromal, congenital forms, the inheritance is most likely autosomal dominant with a high degree of phenotypic variability. Brachydactyly may be associated with short stature, syndactyly, polydactyly, nail hypoplasia or aplasia, and a variety of malformation syndromes. Symphalangism, an autosomal dominant inherited disorder associated with symbrachydactyly or syndactyly, can be both the cause and effect of brachydactyly.54-56 Brachydactyly may also appear with either a longitudinal deficiency, such as radial and ulnar longitudinal deficiencies, or a transverse congenital amputation, such as constriction ring sequence and symbrachydactyly or transverse deficiency (Figure 11).57 It defines a malformation of the hand plate due to abnormal proximal-distal axis differentiation in the updated OMT classification.4
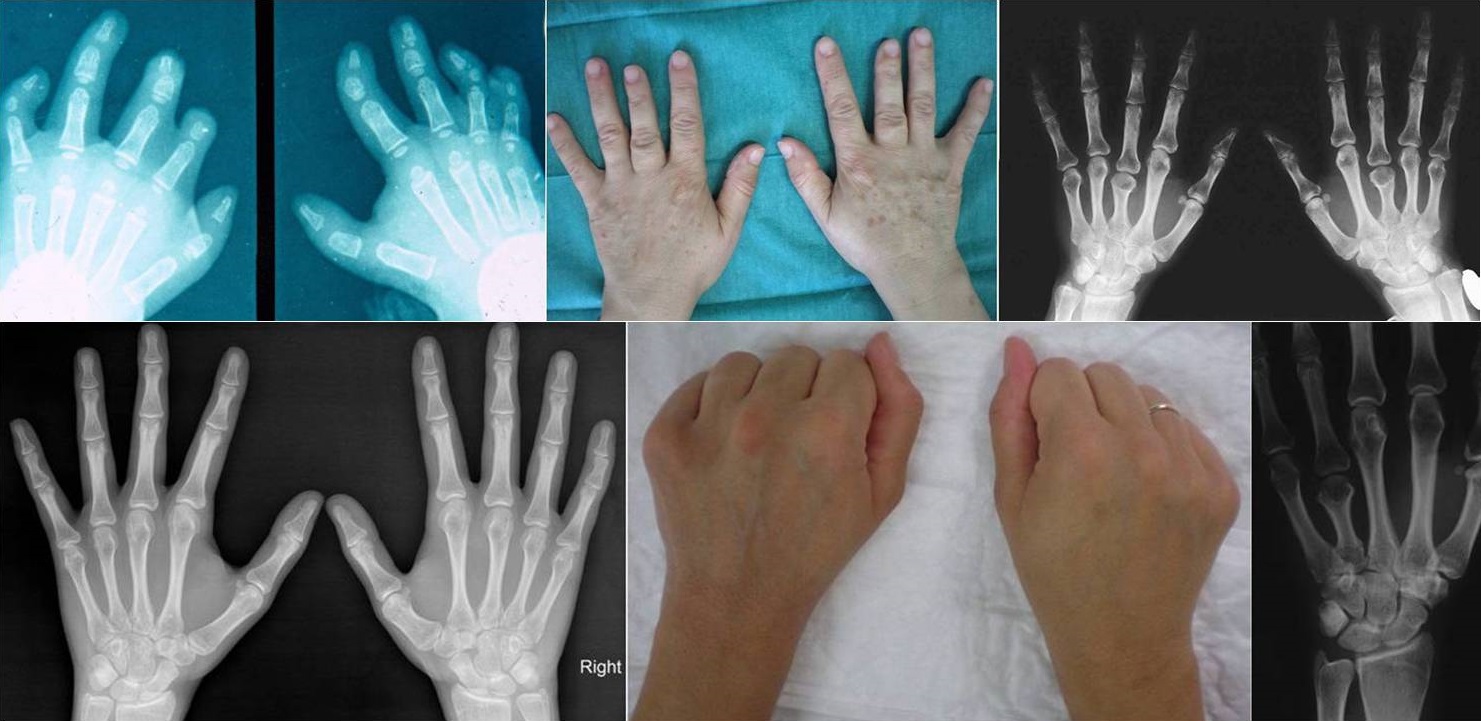
Figure 11. Brachydactyly. (Top left) Bilateral symmetric brachymesophalangia of the 4 ulnar digits and hypoplasia of the thumb’s proximal phalanx of the right hand are evident in a 14-month-old girl. There is an absence of the middle phalanx of the index finger and incomplete cutaneous syndactyly between the index and middle fingers of the left hand. The pediatric evaluation revealed no functional impairment or syndromal disorders. (Top middle and right) The clinical and radiographic appearance of a 52-year-old woman shows isolated bilateral and symmetric shortening of the third finger metacarpal. (Bottom left) Isolated unilateral involvement is evident in a 14-year-old girl with shortening of the right first metacarpal. (Bottom middle and right) A 40-year-old woman was diagnosed with brachymetacarpia of the left ring finger ray.
Revised features on the differential diagnosis of ULD
The literature review showed significantly revised findings regarding the differential diagnosis of ULD. Dwivedi et al reported 14 cases of ULD with bilateral involvement among 75 patients; they indicated that associated medical and musculoskeletal conditions are common in patients with ULD, of which cardiac and lower extremity abnormalities, such as fibular hypoplasia and focal femoral dysplasia, are the most frequent.58 Lowry et al reported that symbrachydactyly can occasionally occur bilaterally; these cases may be misdiagnosed as inherited anomalies such as cleft hand or brachydactyly.19 Furthermore, although brachydactyly is typically a bilateral and symmetric anomaly, some types may appear with asymmetric bilateral or unilateral abnormality.59
Dysplastic ulna
The differential diagnosis of ULD also includes a dysplastic ulna with or without shortening due to congenital anomalies other than transverse deficiency. Congenital bowing of the ulna may be detected in patients suffering from radial clubhand (in cases with a proximal radial remnant, the ulna is thickened, shortened, and bowed radially),60 congenital dislocation of the radial head,61 intraosseous neurofibromas of the ulna,62 hereditary bone dysplasias,63 and aggressive fibromatosis.64
Discussion
In case 1 the differential diagnosis included symbrachydactyly and brachydactyly. The final diagnosis changed from ulnar deficient hand to the short-finger type of symbrachydactyly based on the morphologic characteristics of a hand with hypoplasia of the 4 ulnar fingers with incomplete cutaneous syndactyly, as well as on the radiographic findings. The deformities showed the typical progression of the finger reduction detected in symbrachydactyly from the central to the ulnar digits and from the middle phalanges to all phalanges and metacarpals sequentially. The mild hypoplasia of the proximal phalanx of the thumb is consistent with its embryological origin, equivalent to the middle phalanges of the other digits. These findings are not consistent with ULD or any brachydactyly type.
In case 2, the differential diagnosis of the terminal phalanx of the fifth finger included a distal phalanx (absence of the middle phalanx), a middle phalanx (absence of the distal phalanx) that had assumed the shape of the distal phalanx, and symphalangism due to the presence of a single interphalangeal joint. The absence of the nail or nail remnants of the fifth finger could be erroneously indicative of an absent distal phalanx, consistent with the diagnosis of ulnar deficient hand, terminal transverse deficiency of the hand plate without ectodermal elements, constriction ring sequence, hypodactyly, or brachydactyly-anonychia. The changed diagnosis from ulnar deficient hand to the short-finger type of symbrachydactyly in the context of Poland syndrome was based on the morphologic characteristics of a hand with hypoplasia of the 4 ulnar fingers, the incomplete cutaneous syndactyly, and the radiographic findings of phalangeal and metacarpal hypoplasia of the fingers. The degree of shortening severity of the central middle phalanges increased from the index to the ring finger, indicating that the missing phalanx of the fifth finger was most likely the middle one. However, the nail agenesis of the fifth finger and the sequential progression of shortening from the ulnar to the central digits were not considered consistent with symbrachydactyly. The distal phalanx is never aplastic in the classic hand deformity of Poland syndrome;32 that is consistent with the diagnosed absence of the middle phalanx of the fifth finger in our patient. Symphalangism, although consistent with the diagnosis of symbrachydactyly, was excluded because it is usually associated with a stiff finger due to absent flexor and extensor tendons.65 Patients with Poland syndrome may appear with constriction bands, and nail agenesis has also been previously reported.66 Therefore, anonychia is consistent with the diagnosis of Poland syndrome in our patient. Furthermore, the literature review indicates that any hand anomaly besides symbrachydactyly should be considered indicative of missing associated anomalies and potential Poland syndrome.35 This was evident in our patient, who presented with symbrachydactyly associated with nail aplasia and also proved to suffer from Sprengel’s deformity and thoracic scoliosis, which suggested the final diagnosis of Poland syndrome.
In case 3, a patient who had a congenital anomaly with amputation, the first approach in the differential diagnosis was to consider a potential constriction ring sequence or transverse deficiency. The radiographic appearance of the bowed ulna excluded the diagnosis of ULD, and the dysplastic appearance of both forearm bones proximal to the level of deficiency excluded an amputation due to the constriction ring sequence. The final radiographic diagnosis of upper extremity transverse deficiency at the level of the forearm or segmental transverse deficiency without ectodermal elements also indicated the diagnosis of the 2 deep skin folds at the terminal aspect of the distal stump as soft tissue invaginations of the deficient limb.
In case 4, the misdiagnosis as ULD was due to the shortening of the fifth finger ray secondary to the partial synostosis between the fourth and fifth metacarpal. This type of synostosis usually presents with associated hand anomalies, such as an absent thumb, cleft hand, polysyndactyly, or congenital malformation syndromes. In addition, the findings of hand pattern profiles and dermatoglyphics suggest that the fusion of the fourth and fifth metacarpal should be classified as a failure of separation, rather than a failure of formation or ULD.67 In our patient, independent thumb hypoplasia was excluded because of the synostosis between the fourth and fifth metacarpal and the bilateral posterior congenital dislocation of the radial head. They suggested the final diagnosis of radial longitudinal deficiency because a potential syndromal radial defect had been excluded.
In case 5, the final diagnosis changed from ULD to isolated brachydactyly type E based on the genetic origin, the morphologic characteristics of the patient, and the radiographic findings. Brachydactyly type E may present as an isolated disorder or with malformation syndromes. It results from hypoplastic and partially fused metacarpal epiphyses. The terminal phalanges are often short, hyperextensibility of the hand joints is frequent, and the axial triradius is often relatively high. In addition, affected individuals are slightly short of stature.55 The findings of the patient presented in this study were consistent with a syndrome of a benign nature presenting with hereditary shortening of digits, metacarpals, metatarsals, and long bones referred to as brachydactyly type E.54,68 The only inconsistency in our patient with the latter syndrome was that the right fifth metacarpal was not involved.
In case 6, the final diagnosis changed from ULD to congenital pseudarthrosis of the ulna and osteolysis of its middle diaphyseal third in a patient with NF1; this was based on the dysplastic radiographic configuration of the shortened ulna. The epiphysis of the distal ulnar fragment is always present in congenital pseudarthrosis, although it may not be evident radiographically. On the contrary, hypoplasia of the ulna and underdeveloped fingers may be present, while distal ulnar epiphysis may be absent in ULD.69 Osteolysis presenting as a segmental defect is rare and may be due to periosteal involvement. Misdiagnosis as ULD is inevitable in cases with congenital bowing but without bone distortion, fracture, and destruction, especially in NF1 patients with a missed comprehensive and careful physical examination.70,71
In case 7, the differential diagnosis included acquired (secondary) negative ulnar variance and a potential coexistent congenital syndrome with stenosis of the medullary spaces of the central metacarpals. Congenital negative ulnar variance is a rare anomaly that lacks a family history and more commonly occurs in females than males; it also typically affects both wrists. The mechanism for the development of the anomaly has still not been clarified. It is usually diagnosed in asymptomatic adults and is considered a predisposing factor in the development of ulnar impingement syndrome.72 In a Greek population with minus ulnar variance, a limited number of cases with extreme shortening also exhibited increased obliquity of the distal radial epiphysis.73 Other authors have classified cases with a bilateral shortened and curved distal ulna as mild ULD but not as dysplasia.74 It may be prudent to accept that patients with hypoplasia of the ulna, ulnar styloid, and ulnar head, which are associated with an abnormal bone configuration, should be considered as dysplastic ulna rather than as ULD. The literature review on metacarpal stenosis indicated that, in dwarfism, medullary stenosis in tubular bones is due to cortical thickening,75 most commonly involving the metacarpals and metatarsals, of which the first and fifth are the least affected.76 In brachydactyly, the thinned shaft and broadened epiphyses may complicate the radiographic appearance of the metacarpals and proximal phalanges, giving them an hourglass contour.77 Reduced medullary cavity widths have also been detected in apparently normal individuals.78 In our patient, the lack of any medical or syndromal disorders supported the diagnosis of metacarpal stenosis as a radiographic variant. The final diagnosis changed from ULD to congenital bilateral negative ulnar variance based on the lack of hand anomalies, the normal radiographic appearance of the ulnar head and styloid process, and the bilateral scalloping of the distal radius, which is inconsistent with the diagnosis of ULD. In addition, there was no evidence of rheumatoid arthritis or other inflammatory diseases, and the symmetrical bilateral anomaly excluded a posttraumatic lesion.
This retrospective study revealed the spectrum of the diagnostic overlap of ULD with other anomalies involving the hand plate or the upper limb, the dysplastic ulna, and syndromes. It also indicated the deficits of single-diagnosis documentation of ULD. It may be prudent to consider that patients with congenital anomalies of the hand or upper limb may suffer from additional missing musculoskeletal abnormalities and syndromes until otherwise proven. Furthermore, these patients should be referred to a specialist pediatric department to document a potentially associated anomaly of the limbs or trunk and any medical or syndromal disorders because some anomalies may not be sufficiently apparent to the parents to warrant medical advice or may not be complicated with functional impairment. Finally, the treating clinicians or surgeons should be familiar with the clinical and radiographic features of all potential anomalies and syndromes included in the differential diagnosis process of ULD.
Limitations
There are several limitations in this study to consider when evaluating its value. First, candidate bias may have occurred because a single author performed the whole evaluation. Second, spectrum bias may exist because of the limited number of patients. A multicenter prospective study would be the next step to improve the completeness of documentation and compare the number of patients misdiagnosed as ULD between single-diagnosis documentation and an experienced team's assessment.
Conclusions
The differential diagnosis of ULD includes a spectrum of nonsyndromal genetic or nongenetic congenital upper limb anomalies such as symbrachydactyly (with or without Poland syndrome), transverse deficiency, constriction ring sequence, hypodactyly, cleft hand, radial longitudinal deficiency, brachydactyly, bowing-pseudarthrosis of the ulna, other non-defined lesions such as negative ulnar variance, and a long list of syndrome-related defects. Anomalies with missed or misinterpreted clues from history-taking and clinical or radiographic findings, usually recorded after single diagnosis documentation, may commonly be misdiagnosed as ULD.
Acknowledgments
Author: N.K. Sferopoulos, MD, PhD
Affiliation: 2nd Department of Orthopaedic Surgery, Aristotle University of Thessaloniki, “G. Gennimatas” Hospital, 546 35, Thessaloniki, Greece
Correspondence: N.K. Sferopoulos, MD, PhD, P. Papageorgiou 3, 546 35, Thessaloniki, Greece. E-mail: sferopoulos@yahoo.com
Disclosures: The author disclosed no relevant financial or nonfinancial interests.
References
- Bednar MS, James MA, Light TR. Congenital longitudinal deficiency. J Hand Surg Am. 2009;34(9):1739-1747. doi:10.1016/j.jhsa.2009.09.002
- Bauer AS, Bednar MS, James MA. Disruption of the radial/ulnar axis:congenital longitudinal deficiencies. J Hand Surg Am. 2013;38(11):2293-2302; quiz 2302. doi:10.1016/j.jhsa.2013.03.024
- Sferopoulos NK. New documentation system for ulnar longitudinal deficiency. Eplasty. 2024;24:e3. eCollection 2024.
- Goldfarb CA, Ezaki M, Wall LB, Lam WL, Oberg KC. The Oberg-Manske-Tonkin (OMT) classification of congenital upper extremities: update for 2020. J Hand Surg Am. 2020;45(6):542-547. doi:10.1016/j.jhsa.2020.01.002
- Schwabe GC, Mundlos S. Genetics of congenital hand anomalies. Handchir Mikrochir Plast Chir. 2004;36(2-3):85-97. doi:10.1055/s-2004-817884
- Tonkin MA, Tolerton SK, Quick TJ, et al. Classification of congenital anomalies of the hand and upper limb: development and assessment of a new system. J Hand Surg Am. 2013;38(9):1845-1853. doi:10.1016/j.jhsa.2013.03.019
- Bae DS, Canizares MF, Miller PE, et al. Intraobserver and interobserver reliability of the Oberg-Manske-Tonkin (OMT) classification: establishing a registry on congenital upper limb differences. J Pediatr Orthop. 2018;38(1):69-74. doi:10.1097/BPO.0000000000000732
- Sletten IN, Winge MI, Hülsemann W, Arner M, Hansen KL, Jokihaara J. Inter- and intra-rater reliability of the Oberg-Manske-Tonkin classification of congenital upper limb anomalies. J Hand Surg Eur Vol. 2022;47(10):1016-1024. doi:10.1177/17531934221107264
- Tonkin MA, Oberg KC. The OMT classification of congenital anomalies of the hand and upper limb. Hand Surg. 2015;20(3):336-342. doi:10.1142/S0218810415400055
- Goodell PB, Bauer AS, Sierra FJ, James MA. Symbrachydactyly. Hand (N Y). 2016;11(3):262-270. doi:10.1177/1558944715614857
- Bavinck JN, Weaver DD. Subclavian artery supply disruption sequence: hypothesis of a vascular etiology for Poland, Klippel-Feil, and Möbius anomalies. Am J Med Genet. 1986;23(4):903-918. doi:10.1002/ajmg.1320230405
- Knight JB, Pritsch T, Ezaki M, Oishi SN. Unilateral congenital terminal finger absences: a condition that differs from symbrachydactyly. J Hand Surg Am. 2012;37(1):124-129. doi:10.1016/j.jhsa.2011.09.018
- Al-Qattan MM, Al-Thunyan A. Ulnar deficiencies. In: Abzug MJ, Kozin HS, Zlotolow AD, eds. The Pediatric Upper Extremity. Springer; 2015:265-275. doi:10.1007/978-1-4614-8515-5_12
- Wall LB, McCombe D, Goldfarb CA, Lam WL; ICHAD study group. The Oberg, Manske, and Tonkin classification of congenital upper limb anomalies: a consensus decision-making study for difficult or unclassifiable cases. J Hand Surg Am. 2024;49(4):379.e1-379.e7. doi:10.1016/j.jhsa.2022.07.007
- Baek GH, Kim J. Oligodactyly with thumb. J Hand Surg Asian Pac Vol. 2016;21(3):283-291. doi:10.1142/S2424835516400087
- Cole RJ, Manske PR. Classification of ulnar deficiency according to the thumb and first web. J Hand Surg Am. 1997;22(3):479-488. doi:10.1016/S0363-5023(97)80016-0
- Ogino T, Saitou Y. Congenital constriction band syndrome and transverse deficiency. J Hand Surg Br. 1987;12(3):343-348. doi:10.1016/0266-7681_87_90185-9
- Tonkin MA. Classification of congenital anomalies of the hand and upper limb. J Hand Surg Eur Vol. 2017;42(5):448-456. doi:10.1177/1753193417690965
- Lowry RB, Bedard T, Kiefer GN, Sass KR. Views on the Oberg-Manske-Tonkin classification system for congenital anomalies of the hand and upper limb. J Hand Surg Am. 2017;42(5):378-381. doi:10.1016/j.jhsa.2017.02.018
- Holmes LB, Nasri HZ. Hypothesis: symbrachydactyly. Am J Med Genet A. 2022;188(11):3236-3241. doi:10.1002/ajmg.a.62941
- Buck-Gramcko D. Symbrachydactyly: a clinical entity. Tech Hand Up Extrem Surg. 1999;3(4):242-258.
- Woodside JC, Light TR. Symbrachydactyly-diagnosis, function, and treatment. J Hand Surg Am. 2016;41(1):135-143; quiz 143. doi:10.1016/j.jhsa.2015.06.114
- Kallemeier PM, Manske PR, Davis B, Goldfarb CA. An assessment of the relationship between congenital transverse deficiency of the forearm and symbrachydactyly. J Hand Surg Am. 2007;32(9):1408-1412. doi:10.1016/j.jhsa.2007.08.011
- Yamauchi Y, Tanabu S. Symbrachydactyly. In: Buck-Gramcko D, ed. Congenital Malformations of the Hand and Forearm. Churchill Livingstone; 1998:149-158.
- Goodell PB, Bauer AS, Oishi S, et al. Functional assessment of children and adolescents with symbrachydactyly: a unilateral hand malformation. J Bone Joint Surg Am. 2017;99(13):1119-1128. doi:10.2106/JBJS.16.01283
- Foucher G, Medina J, Pajardi G, Navarro R. La symbrachydactylie, classification et traitement. A propos d'une série de 117 cas [Classification and treatment of symbrachydactyly. A series of 117 cases]. Chir Main. 2000;19(3):161-168. doi:10.1016/s1297-3203(00)73475-5
- Jones NF, Kaplan J. A new documentation system for congenital absent digits. Hand (N Y). 2012;7(4):391-399. doi:10.1007/s11552-012-9450-0
- Hu CH, Ray LJ, Bae DS, Goldfarb CA, James MA, Van Heest AE; CoULD Study Group. Do nails and nubbins matter? A comparison of symbrachydactyly and transverse deficiency phenotypes. J Hand Surg Am. 2024;49(11):1136.e1-1136.e9. doi:10.1016/j.jhsa.2023.01.021
- Holmes LB, Nasri HZ. Hypothesis: central digit hypoplasia. Am J Med Genet A. 2022;188(6):1746-1751. doi:10.1002/ajmg.a.62697
- Ireland DC, Takayama N, Flatt AE. Poland’s syndrome. J Bone Joint Surg Am. 1976;58(1):52-58.
- Tafti D, Cecava ND. Poland Syndrome. 2023 May 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–.
- Al-Qattan MM, Al Thunayan A. The middle phalanx in Poland syndrome. Ann Plast Surg. 2005;54(2):160-164. doi:10.1097/01.sap.0000143863.52037.dc
- Catena N, Divizia MT, Calevo MG, et al. Hand and upper limb anomalies in Poland syndrome: a new proposal of classification. J Pediatr Orthop. 2012;32(7):727-731. doi:10.1097/BPO.0b013e318269c898
- Buckwalter JA V, Shah AS. Presentation and treatment of Poland anomaly. Hand (N Y). 2016;11(4):389-395. doi:10.1177/1558944716647355
- Baas M. Above and beyond: classification of congenital upper limb anomalies. Thesis. Erasmus University Rotterdam. 2021;83-103. http://hdl.handle.net/1765/135709. Accessed March 28, 2025.
- Kozin SH. Upper-extremity congenital anomalies. J Bone Joint Surg Am. 2003;85(8):1564-1576. doi:10.2106/00004623-200308000-00021
- Swanson AB. A classification for congenital limb malformations. J Hand Surg Am. 1976;1(1):8-22. doi:10.1016/s0363-5023(76)80021-4
- Kawamura K, Chung KC. Constriction band syndrome. Hand Clin. 2009;25(2):257-264. doi:10.1016/j.hcl.2008.10.007
- Goldfarb CA, Sathienkijkanchai A, Robin NH. Amniotic constriction band: a multidisciplinary assessment of etiology and clinical presentation. J Bone Joint Surg Am. 2009;91 Suppl 4:68-75. doi:10.2106/JBJS.I.00339
- Buchler U. Symbrachydactyly. In: Gupta A, Kay SPJ, Scheker LR, eds. The Growing Hand: Diagnosis and Management of The Upper Extremity in Children. Mosby Harcourt Publishers Limited, London; 2000:213-223.
- Ogino T. Clinical features and teratogenic mechanisms of congenital absence of digits. Dev Growth Differ. 2007;49(6):523-531. doi:10.1111/j.1440-169X.2007.00939.x
- Davis DD, Kane SM. Cleft Hand. 2023 Aug 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–.
- Tonkin MA. Commentary on “Views on the Oberg-Manske-Tonkin classification system for congenital anomalies of the hand and upper limb”. J Hand Surg Am. 2017;42(5):382-384. doi:10.1016/j.jhsa.2017.02.019
- Guero S, Holder-Espinasse M. Insights into the pathogenesis and treatment of split/hand foot malformation (cleft hand/foot). J Hand Surg Eur Vol. 2019;44(1):80-87. doi:10.1177/1753193418807375
- Ogino T. Teratogenic relationship between polydactyly, syndactyly and cleft hand. J Hand Surg Br. 1990;15(2):201-209. doi:10.1016/0266-7681_90_90125-n
- Ogino T. Teratogenic mechanisms of longitudinal deficiency and cleft hand. Handchir Mikrochir Plast Chir. 2004;36(2-3):108-116. doi:10.1055/s-2004-817872
- Iba K, Horii E, Ogino T, Kazuki K, Kashiwa K; Congenital Hand Committee of Japanese Society for Surgery of the Hand. The classification of Swanson for congenital anomalies of upper limb modified by the Japanese Society for Surgery of the Hand (JSSH). Hand Surg. 2015;20(2):237-250. doi:10.1142/S0218810415300041
- Soldado F, Zlotolow DA, Kozin SH. Thumb hypoplasia. J Hand Surg Am. 2013;38(7):1435-1444. doi:10.1016/j.jhsa.2013.03.021
- Dy CJ, Swarup I, Daluiski A. Embryology, diagnosis, and evaluation of congenital hand anomalies. Curr Rev Musculoskelet Med. 2014;7(1):60-67. doi:10.1007/s12178-014-9201-7
- Pfeiffer RA, Santelmann R. Limb anomalies in chromosomal aberrations. Birth Defects Orig Artic Ser. 1977;13(1):319-337.
- Wall LB, Ezaki M, Oishi SN. Management of congenital radial longitudinal deficiency: controversies and current concepts. Plast Reconstr Surg. 2013;132(1):122-128. doi:10.1097/PRS.0b013e318290fca5
- James MA, McCarroll HR Jr, Manske PR. Characteristics of patients with hypoplastic thumbs. J Hand Surg Am. 1996;21(1):104-113. doi:10.1016/s0363-5023(96)80162-6
- James MA, McCarroll HR Jr, Manske PR. The spectrum of radial longitudinal deficiency: a modified classification. J Hand Surg Am. 1999;24(6):1145-1155. doi:10.1053/jhsu.1999.1145
- Fitch N. Classification and identification of inherited brachydactylies. J Med Genet. 1979;16(1):36-44. doi:10.1136/jmg.16.1.36
- Temtamy SA, Aglan MS. Brachydactyly. Orphanet J Rare Dis. 2008;3:15. doi:10.1186/1750-1172-3-15
- Gottschalk MB, Danilevich M, Gottschalk HP. Carpal coalitions and metacarpal synostoses: a review. Hand (N Y). 2016;11(3):271-277. doi:10.1177/1558944715614860
- Nguyen ML, Jones NF. Undergrowth: brachydactyly. Hand Clin. 2009;25(2):247-255. doi:10.1016/j.hcl.2009.02.003
- Dwivedi N, Goldfarb CA, Bauer A, Bohn D, Samora JB, Wall LB; CoULD Study Group. An analysis of associated conditions and the relationship between the severity of hand manifestations with that of the forearm in ulnar longitudinal deficiency. J Hand Surg Am. 2024;49(2):180.e1-180.e9. doi:10.1016/j.jhsa.2022.05.021
- Robin NH, Hurvitz J, Warman ML, Morrison S. Clinical and molecular studies of brachydactyly type D. Am J Med Genet. 1999;85(4):413-418. doi:10.1002/(sici)1096-8628(19990806)85:4<413::aid-ajmg20>3.0.co;2-c
- Bayne LG, Klug MS. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg Am. 1987;12(2):169-179. doi:10.1016/s0363-5023(87)80267-8
- Good CJ, Wicks MH. Developmental posterior dislocation of the radial head. J Bone Joint Surg Br. 1983;65(1):64-65. doi:10.1302/0301-620X.65B1.6822604
- Baldwin DM, Weiner DS. Congenital bowing and intraosseous neurofibroma of the ulna. A case report. J Bone Joint Surg Am. 1974;56(4):803-807.
- Rosenberg E, Löhr H. A new hereditary bone dysplasia with characteristic bowing and thickening of the distal ulna. Eur J Pediatr. 1986;145(1-2):40-45. doi:10.1007/BF00441850
- Eady JL, Lundquist JE, Grant RE, Nagel A, Kim DD. Congenital bowing of the ulna and aggressive fibromatosis. J Natl Med Assoc. 1991;83(11):978-982.
- Jose R, O’Brien M, Burke F. Congenital hand anomalies. In: Bentley G, ed. European Surgical Orthopaedics and Traumatology. Springer; 2014:1653-1673. doi:10.1007/978-3-642-34746-7_87
- Senrui H, Egawa T, Horiki A. Anatomical findings in the hands of patients with Poland's syndrome. J Bone Joint Surg Am. 1982;64(7):1079-1082.
- Miura T. Congenital synostosis between the fourth and fifth metacarpal bones. J Hand Surg Am. 1988;13(1):83-88. doi:10.1016/0363-5023(88)90206-7
- Riccardi VM, Holmes LB. Brachydactyly, type E: hereditary shortening of digits, metacarpals, metatarsals, and long bones. J Pediatr. 1974;84(2):251-254. doi:10.1016/s0022-3476(74)80614-1
- Cheng JC, Hung LK, Bundoc RC. Congenital pseudarthrosis of the ulna. J Hand Surg Br. 1994;19(2):238-243. doi:10.1016/0266-7681(94)90176-7
- Maffulli N, Fixsen JA. Pseudoarthrosis of the ulna in neurofibromatosis. A report of four cases. Arch Orthop Trauma Surg. 1991;110(4):204-207. doi:10.1007/BF00571060
- Shen Y, Chen F. Unusual form of the distal bone defect of ulna with neurofibromatosis type 1: a case report. Medicine (Baltimore). 2019;98(40):e17226. doi:10.1097/MD.0000000000017226
- Voorhees DR, Daffner RH, Nunley JA, Gilula LA. Carpal ligamentous disruptions and negative ulnar variance. Skeletal Radiol. 1985;13(4):257-262. doi:10.1007/BF00355345
- Lyritis G, Dimitracopoulos B, Nikolaou P, Gorgolis J. Functional disturbance of the inferior radio-ulnar joint due to hypoplasia of the lower end of the ulna. Prog Clin Biol Res. 1982;104:339-344.
- Farr S, Schachinger F. Treatment of mild ulnar longitudinal deficiency with a z-shaped ulna lengthening osteotomy: a report of 2 cases. JBJS Case Connect. 2020;10(3):e20.00080. doi:10.2106/JBJS.CC.20.00080
- Kenny FM, Linarelli L. Dwarfism and cortical thickening of tubular bones. Transient hypocalcemia in a mother and son. Am J Dis Child. 1966;111(2):201-207. doi:10.1001/archpedi.1966.02090050133013
- Caffey J. Congenital stenosis of medullary spaces in tubular bones and calvaria in two proportionate dwarfs--mother and son; coupled with transitory hypocalcemic tetany. Am J Roentgenol Radium Ther Nucl Med. 1967;100(1):1-11. doi:10.2214/ajr.100.1.1
- Itlis H. A new case of typical brachydactyly. J Hered. 1944;35:145-148.
- Garn SM, Davila GH, Rohmann CG. Population frequencies and altered remodeling mechanisms in normal medullary stenosis. Am J Phys Anthropol. 1968;29(3):425-428. doi:10.1002/ajpa.1330290316