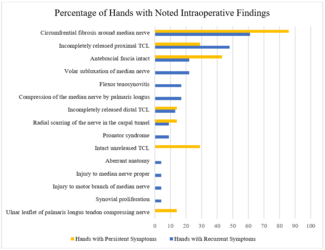
Thoracic Outlet Syndrome: An Overlooked Diagnosis in the Pediatric Population
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Thoracic outlet syndrome (TOS) results from the compression of the brachial plexus and/or subclavian vessels. The diagnosis of this disorder in children is often overlooked because of the mistaken assumption that the disorder does not affect children. There is a lack of knowledge concerning the etiology, treatment, and long-term results of this pathology among younger patients.
We present a case of a 14-year-old girl with paresthesia and weakness of the upper right limb due to an ipsilateral cervical rib. The severity of her complaints motivated the use of surgical decompression by the supraclavicular approach. After a 6-month follow-up period and after an active rehabilitation and strength training program, the patient was free of symptoms.
Thoracic outlet syndrome etiology, treatment choices, and outcomes in the pediatric population remain debatable. Conservative treatment is steered mainly to improving the patient’s posture during the activities of daily living by mitigating the compression on the brachial plexus. Surgical decompression is the treatment of choice for patients with persistent significant symptoms.
Introduction
Thoracic outlet syndrome (TOS) is a designation for a variety of symptoms resulting from the compression of the brachial plexus and/or subclavian vessels.1 It typically affects middle-aged women and in most cases involves the lower inferior trunk of the brachial plexus.2 Although most patients with TOS are adults, it also occurs in the pediatric population; however, the diagnosis of this disorder in children is often overlooked because of the mistaken assumption that the disorder does not affect children.3,4
In adults, TOS is usually characterized by pain in the affected upper limb, weakness, abnormal sensitivity to cold, and hand paresthesia. Atrophy of the thenar and hypothenar eminences may also be present. On the other hand, children with TOS generally complain of neck soreness, upper limb hypoesthesia, and decreased muscle strength.5
TOS can be caused by cervical ribs, abnormal first ribs, congenital bands, masses in the thoracic outlet, trauma, or repetitive motions.3,4,6 Differential diagnosis includes brachial plexus injuries, cervical spine lesions, shoulder impingement syndrome, and distal overuse injuries, among others.
There is a lack of knowledge concerning the etiology, treatment, and long-term results of this pathology amid younger patients. Here, we present a case of a 14-year-old girl with paresthesia and weakness of the upper right limb due to an ipsilateral cervical rib.
Case Presentation
A 14-year-old girl was referred to our clinic because of paresthesia and weakness of the upper right limb. She had experienced these symptoms since she was 10 years old.
Upon physical examination, our patient presented with neck discomfort, right neck swelling, upper right limb numbness, muscular strength grade of 4-, and hypoesthesia of the fourth and fifth ipsilateral fingers. Her cervical ribs were palpable bilaterally, but more obvious on the right side.
The hyperabduction maneuver (Wright test) showed no change in the radial pulse. The Adson test was also negative. Light percussion of the cubital nerve in the wrist caused a tingling sensation, which is a positive Hoffman sign. The cervical spine X-ray showed bilateral cervical ribs, more evident on the right side (Figure 1).
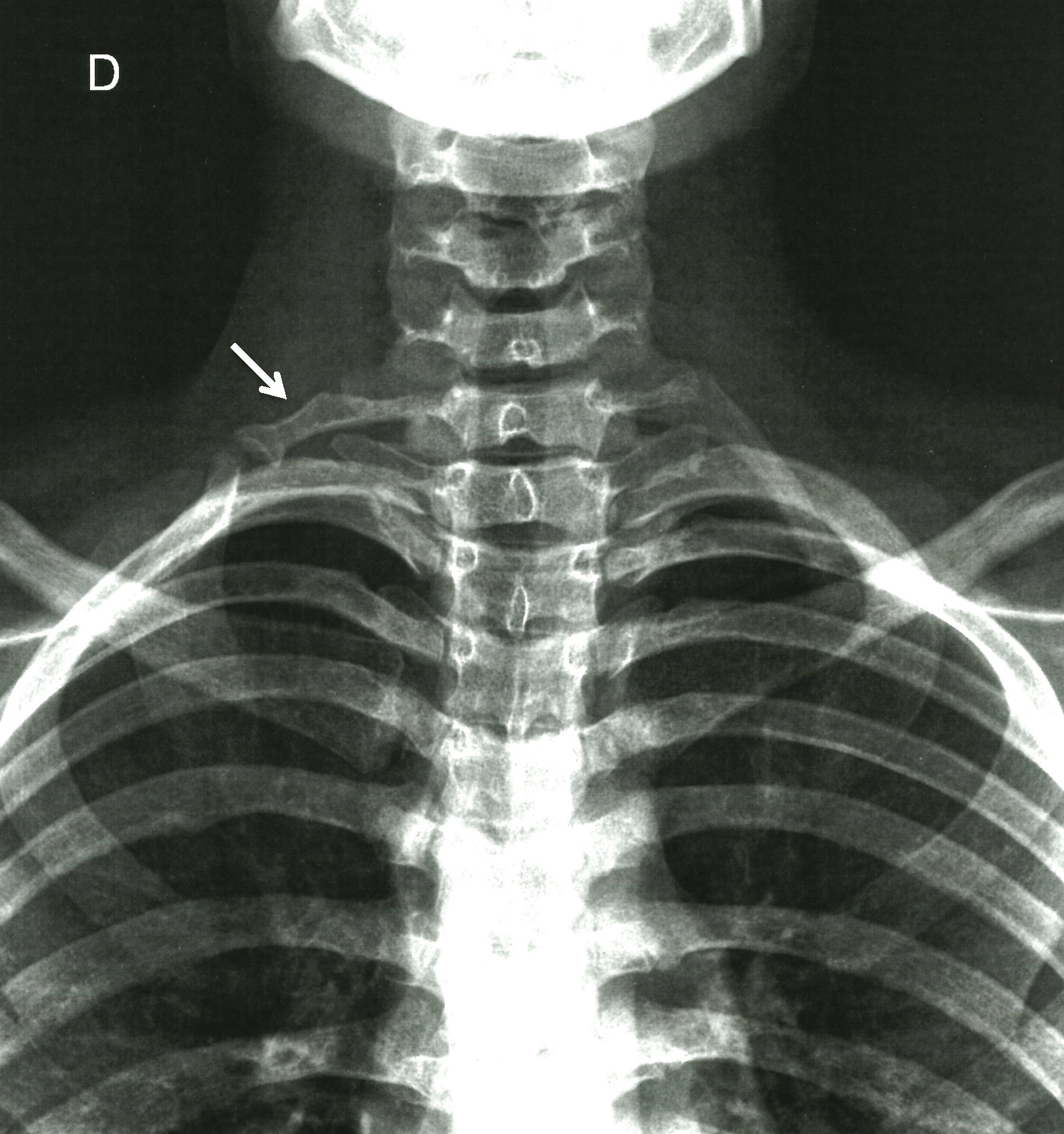
Figure 1. Anteroposterior X-ray film of the cervical spine showing bilateral cervical ribs more evident on the right side (arrow).
Electromyography revealed a reduction in the sensitivity responses of the right medial antebrachial cutaneous and ulnar nerves, a reduced number of F responses of the right median nerve, and an increased latency of the F responses of the right ulnar nerve. No changes were found on the sensitive or motor conduction on the left side. The computed tomography scan showed the presence of cervical ribs on C7, larger on the right side, which articulated with the top of the first costal arch (Figure 2).
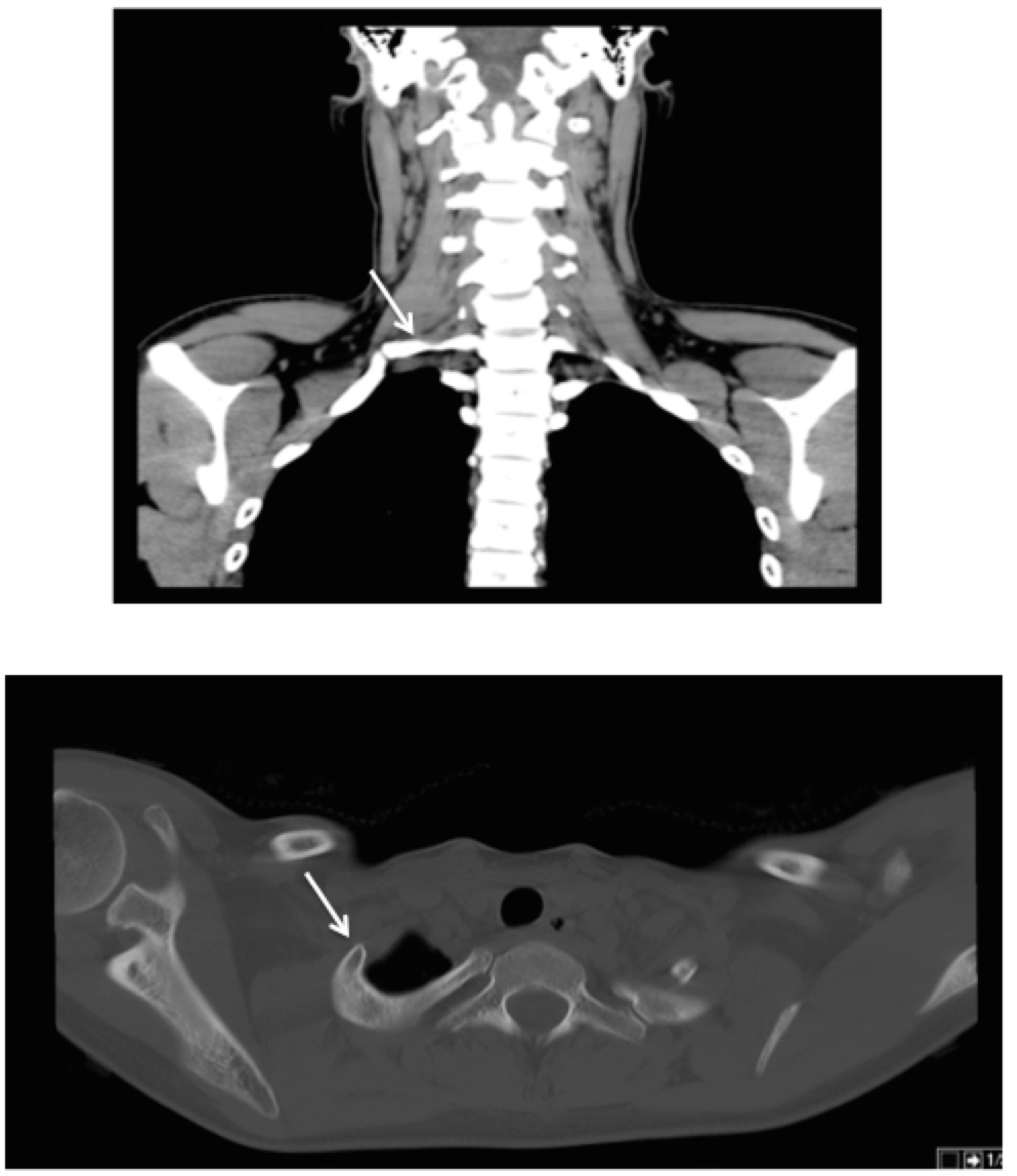
Figure 2. Computed tomography scan showing the C7 cervical ribs (arrows), larger on the right side, with an initial segment with a posterolateral orientation and a distal segment with a anterolateral orientation, which articulates with the top of the first costal arch. Upper image: coronal view; lower image: axial view.
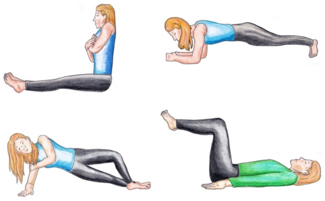
A conservative approach was attempted initially, including patient education and rehabilitation. In addition to specific physical therapy, the patient was advised to rest and avoid excessive physical activity, to keep adequate posture, and to perform some brachial plexus relaxing maneuvers at home. This approach did not improve her symptoms within the first 6 months and she was reluctant to undergo nerve block with injectable local anesthetics. Because these symptoms were affecting her quality of life, a surgical treatment was discussed with our patient and her parents, to which they consented.
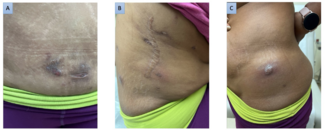
A supraclavicular approach to decompress the brachial plexus and to remove the first rib was undertaken. To begin the procedure, the patient was placed in the supine position. A sandbag was placed between the scapulae, and the neck was extended to the nonoperative side. An incision was made in the supraclavicular fossa, parallel to and 2 cm above the clavicle (Figure 3). The supraclavicular nerves were identified beneath the platysma and mobilized. The omohyoid and the lateral portion of the clavicular head of the sternocleidomastoid (SCM) muscles were divided. The phrenic and long thoracic nerves were identified and protected.

Figure 3. Preoperative markings: an incision was made in the supraclavicular fossa, parallel to and 2 cm above the clavicle (dotted line).
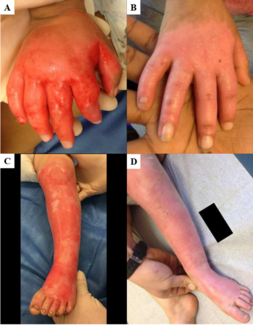
Next, the anterior and middle scalene muscles were divided from the first rib. The 3 trunks of the brachial plexus were visualized and gently protected. A supernumerary anomalous rib with a 90-degree curvature was unveiled, which was articulated to the first costal arch. Compression of the inferior trunk of the brachial plexus and the subclavian artery was obvious (Figure 4). The first rib was encircled and divided (Figure 5). It was decided not to remove the posterior edge of the first rib because of the iatrogenic risk of C8 root damage. The SCM muscle was repaired, and the wound was closed in a subcuticular fashion over a suction drain. The postoperative period was uneventful, and the patient was discharged home on the third day postoperative.
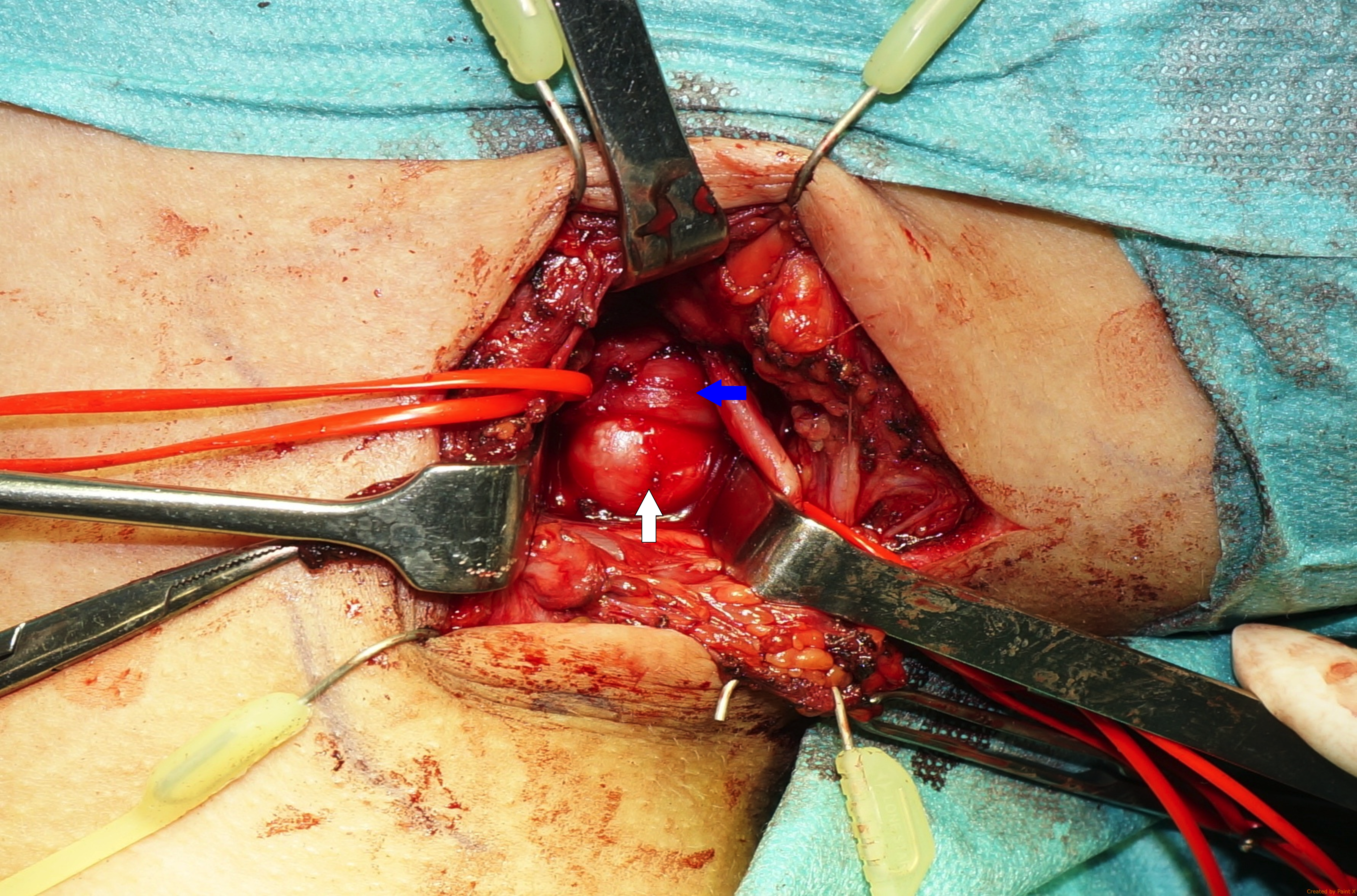
Figure 4. The supernumerary anomalous rib with a 90-degree curvature articulated to the first costal arch. A compression of the inferior trunk of the brachial plexus is evident. White arrow: anomalous rib; blue arrow: inferior trunk.
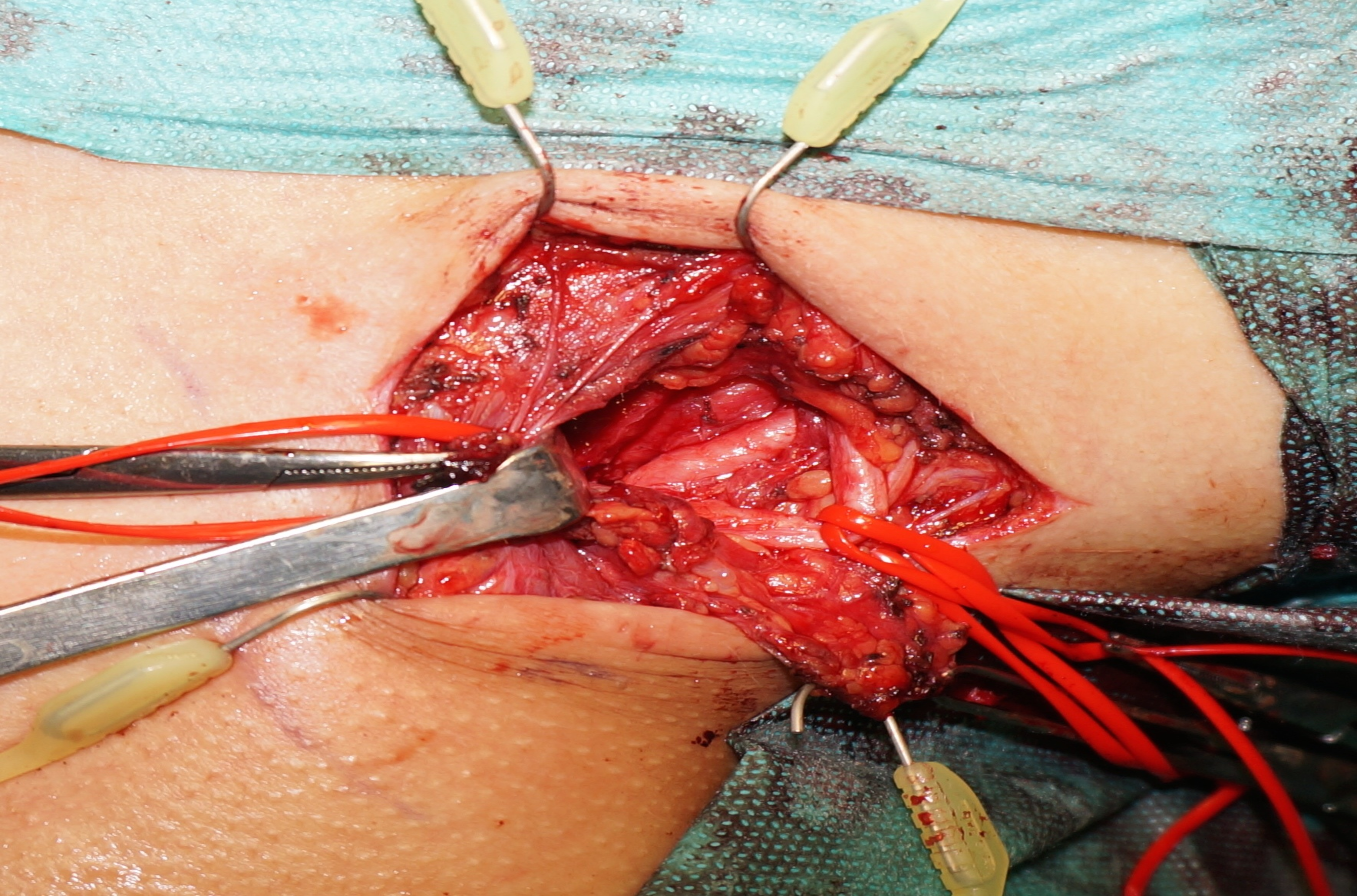
Figure 5. After division of the first rib: note the normal anatomical position of the inferior trunk at the end of the surgery.
At the first postoperative outpatient consultation (1-week post-surgery), the patient still complained of hypoesthesia of the fourth and fifth fingers of the right hand, but with an improvement over the preoperative status. Two weeks after surgery, the patient had no complaints, and the neurologic examination was normal. She was able to return to school 12 days after the surgery.
Discussion
TOS includes an array of conditions associated with the compression of the neurovascular structures as they pass through the thoracic outlet. Its etiology, treatment choices, and outcomes in the pediatric population remain debatable. A conservative approach is the first line of treatment and involves patient education and physical therapy.6 Surgical decompression is the treatment of choice for patients who continue to exhibit persistent, significant symptoms after 3 to 6 months of treatment with the conservative approach.6,7,8 In our case, the severity of the patient’s complaints motivated surgical decompression by the supraclavicular approach. After a 6-month follow-up period and an active rehabilitation and strength training program, the patient was free of symptoms.
Conclusions
Despite occurring more frequently in adults, TOS also arises in young children and teenagers but is often misdiagnosed. TOS should be considered in cases where a child complains of neck and shoulder discomfort, hand numbness, and upper limb weakness. Early diagnosis is essential, as diagnostic and treatment delays may lead to significant morbidity. The physical examination is vital for the diagnosis of pediatric TOS. Surgical treatment should be performed if conservative measures are unsuccessful.
Acknowledgments
Authors: Margarida Mendes, MD1; Ricardo Nascimento, MD2; Ricardo Horta, MD, PhD1; Eurico Norton, MD3; Álvaro Silva, MD1
Affiliations: 1Department of Plastic, Reconstructive and Aesthetic Surgery and Burn Unit, Unidade Local de Saúde de São João, Porto, Portugal; 2Department of Plastic, Reconstructive and Aesthetic Surgery, Unidade Local de Saúde de Matosinhos, Porto, Portugal; 3Department of Angiology and Vascular Surgery, Unidade Local de Saúde de São João, Porto, Portugal
Correspondence: Margarida Mendes, MD; margarida_mendes900@hotmail.com
Ethics statement: The patient consented to the use of images.
Disclosures: The authors disclosed no financial or other conflicts of interest.
References
1. Buller LT, Jose J, Baraga M, Lesniak B. Thoracic outlet syndrome: current concepts, imaging features, and therapeutic strategies. Am J Orthop (Belle Mead NJ). 2015;44(8):376-382.
2. Braun RM. Thoracic outlet syndrome: a primer on objective methods of diagnosis. J Hand Surg Am. 2010;35(9):1539-1541; quiz 1541. doi:10.1016/j.jhsa.2010.03.018
3. Maru S, Dosluoglu H, Dryjski M, Cherr G, Curl GR, Harris LM. Thoracic outlet syndrome in children and young adults. Eur J Vasc Endovasc Surg. 2009;38(5):560-564. doi:10.1016/j.ejvs.2009.06.015
4. Arthur LG, Teich S, Hogan M, Caniano DA, Smead W. Pediatric thoracic outlet syndrome: a disorder with serious vascular complications. J Pediatr Surg. 2008;43(6):1089-1094. doi:10.1016/j.jpedsurg.2008.02.038
5. Chang K, Graf E, Davis K, Demos J, Roethle T, Freischlag JA. Spectrum of thoracic outlet syndrome presentation in adolescents. Arch Surg. 2011;146(12):1383-1387. doi:10.1001/archsurg.2011.739
6. Jones MR, Prabhakar A, Viswanath O, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5-18. doi:10.1007/s40122-019-0124-2
7. Chan KH, Gitomer SA, Perkins JN, Liang C, Strain JD. Clinical presentation of cervical ribs in the pediatric population. J Pediatr. 2013;162(3):635-636. doi:10.1016/j.jpeds.2012.10.048
8. Boglione M, Ortíz R, Teplisky D, et al.. Surgical treatment of thoracic outlet syndrome in pediatrics. J Pediatr Surg. 2022;57(9):29-33. doi:10.1016/j.jpedsurg.2021.08.017