Extreme Injury of Multiple Hand Extensor Tendons (Zones II to VII) Combined With an Extensive Degloving Injury of the Dorsal Hand: Staged Reconstruction Utilizing Silicon Rods and a Groin Flap
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Extensive injuries of hand extensor tendons combined with soft tissue loss represent a reconstructive challenge. Single- or multiple-stage reconstruction cannot be principally adopted, and a single surgical plan cannot uniformly treat every patient.
Methods. The authors present a complex case of dorsal hand degloving injury accompanied by extensor tendons injury of the second, third, and fourth digits in zones II to VII, as well as radial wrist extensor tendons injury. The patient was treated in stages. Coverage was provided by a pedicled groin flap. Radial wrist extensors were reconstructed with a palmaris tendon graft, and the extensor digitorum communis was reconstructed with silicon rods and fascia lata grafts.
Conclusions. A most satisfactory reconstruction was achieved.
Introduction
Extensive dorsal hand defects combined with extensor tendons injury are challenging to reconstruct. The surgical team has various parameters to consider before deciding on the operative plan. Single- vs multiple-stage reconstruction, the timing of each surgical step, the type of flap, and the type of tendon graft are some of the factors that must be examined. We present a difficult case that was treated in stages with a favorable result.
Case Presentation
A 50-year-old man was admitted to our hospital because of extensive, composite dorsal trauma to his left hand. He was injured at work while handling an industrial cotton cutting machine. The patient was right-handed, a nonsmoker, and did not have any known comorbidities. During the initial assessment, his radial and ulnar pulses were palpable. Areas of radial nerve distribution were insensate, but the sensory neurological examination was normal for areas innervated by the ulnar and median nerves.
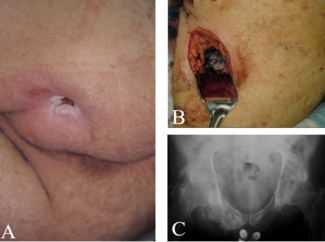
The patient had sustained a degloving injury with soft tissue loss extending from the wrist to the metacarpophalangeal joints (MCP) and extensive lacerations involving the dorsal aspect of the second, third, and fourth digits and the ulnar surface of the thumb. The dorsal surface of the diaphyses of the second, third, and fourth metacarpals was also scraped (Figure 1).
Figure 1. Extensive degloving injury of the dorsal surface of the hand.
The extensor apparatus was heavily traumatized. The second, third, and fourth extensor compartments were deroofed. The extensor digitorum communis (EDC) tendon gap of the first, second, third, and fourth digits extended from zones II to VII. The extensor carpi radialis longus (ECRL) and brevis (ECRB) tendons were destroyed from the level of the wrist to their insertion. The extensor pollicis longus (EPL) and extensor digiti minimi (EDM) were intact.
Because of the severity and the complexity of the trauma, the surgical team opted for a staged reconstruction. During the first operation, a radical debridement was performed. The dorsal surface of the hand was covered with an ipsilateral pedicled groin flap, while the lacerated surfaces of the first, second, third, and fourth digits were treated with tissue rearrangement. Small areas were left to heal by secondary intention (Figure 2). Three weeks later, the pedicle was divided, and the patient followed an aggressive physiotherapy protocol in order to obtain a satisfactory range of motion (ROM). After approximately 2 weeks, the patient underwent his third operation. The ECRB and ECRL tendons were reconstructed with the use of an ipsilateral palmaris longus tendon graft. The 2 tendons were sutured together and weaved with the tendon graft. The distal end was fixated to the base of the second metacarpal through a small, drilled hole (Figure 3). With the help of liposuction cannulas, 4-mm wide silicon rods were placed over the dorsum of the second, third, and fourth metacarpals and digits. The distal ends of the rods were sutured to the remaining stump of the extensor tendon at the level of the middle phalange; the proximal ends were not sutured (Figure 4). The short proximal stump of the EDC was recognized and marked with a suture for future reconstruction. Postoperatively, the hand was immobilized with the wrist in 40° extension, the MCP in 90° flexion, and the finger joints were kept in 0° degrees of flexion for 2 weeks until the wounds healed. Then, the plaster was replaced with a dynamic splint permitting active flexion and passive extension (Figure 5).

Figure 2. Pedicled groin flap for coverage of the dorsal hand.
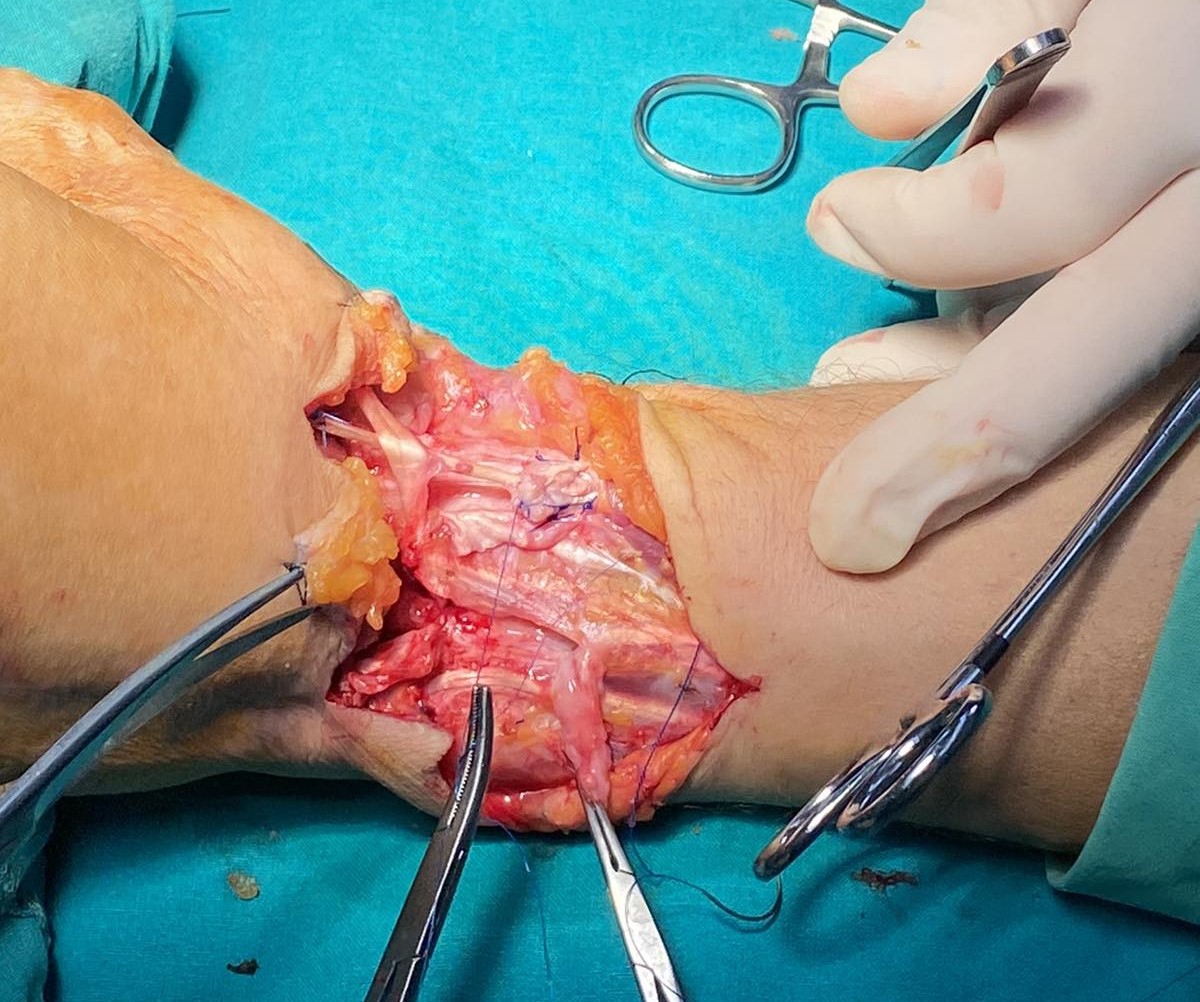
Figure 3. Reconstruction of the extensor carpi radialis longus and brevis.
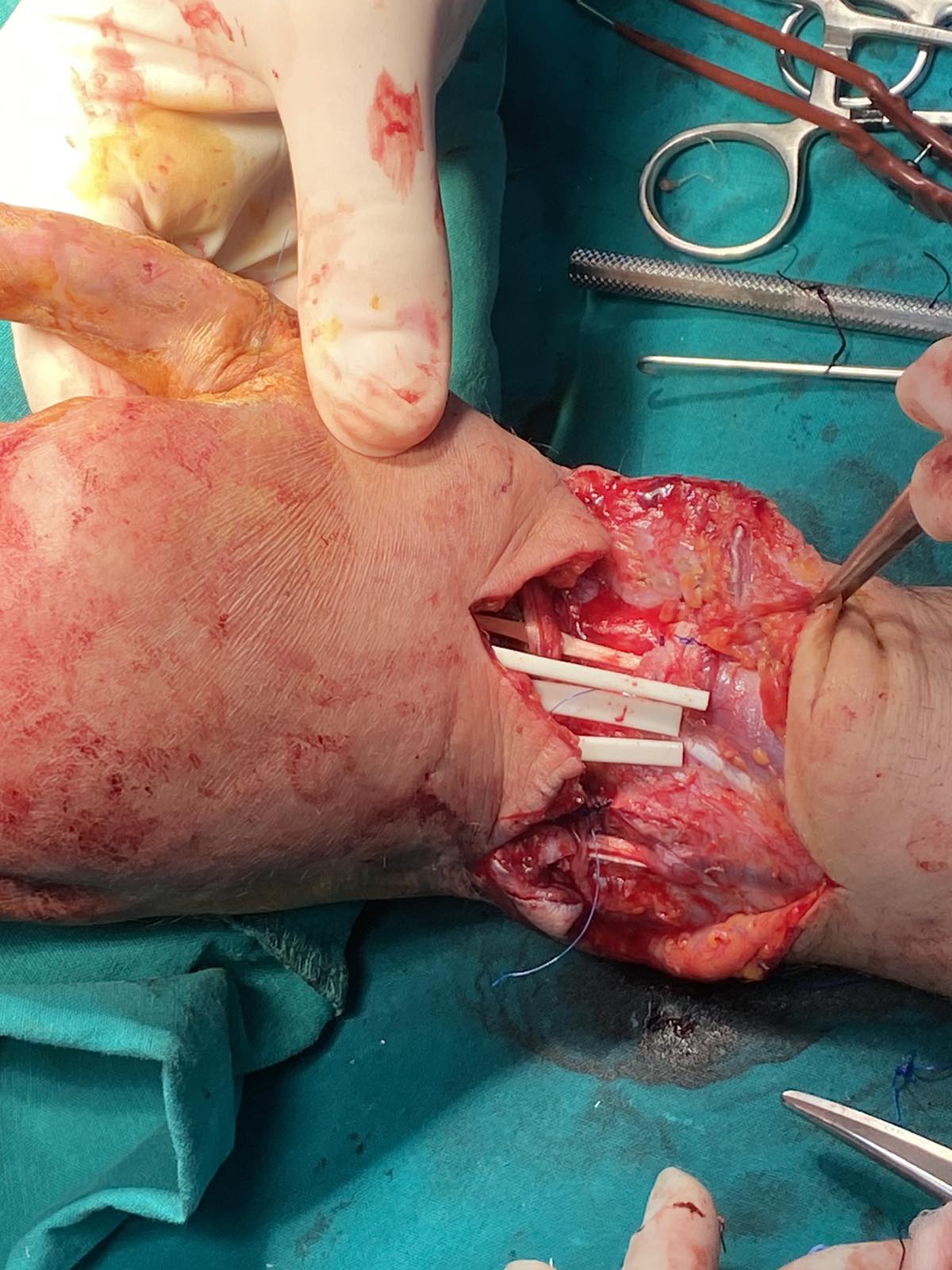
Figure 4. Placement of silicone rods. The proximal end was left free.

Figure 5. Dynamic splint-assisted wrist and finger extension.
From weeks 2 to 4, the wrist was passively extended and actively flexed until straight (0°) and the fingers were fully mobilized. From weeks 4 to 6, active extension of the wrist was initiated (up to 30°). After the sixth week, progressively full ROM of the wrist with active flexion and extension was initiated. Three months later, the fourth and final operation was performed. First, 3 strips of fascia lata, 2-cm wide and 20-cm long, were harvested with a minimally invasive technique using a tendon stripper. The silicon rods were then removed and the fascia lata grafts were inserted through the well-formed pseudosynovial sheaths. Next, with the hand placed in the intrinsic plus position, the distal ends were sutured to the remnants of the extensor tendons while the proximal ends were weaved to the EDC proximal stump.
During the first postoperative week, the hand was immobilized with the wrist in 30° extension and the MCPs and finger joints fully extended. A dynamic splint was applied 7 days postoperatively. From week 1 to week 3, wrist flexion and extension were initiated and the fingers were flexed up to 30° while the wrist was kept straight. From week 3 to week 6, active finger extension was started. From week 6 onward, progressively full flexion of the fingers was pursued.
The patient’s progress was reassessed every 2 weeks during the first 6-week period to ensure normal wound healing and compliance with the physiotherapy guidelines. The patient was reassessed again 3 months after the final operation, and then yearly follow-up visits were performed until the fourth postoperative year.
Favorable wrist and finger active extension up to the level of the pip joints was achieved approximately 1 year after the initial injury. There was no sign of bow stringing over the wrist joint. Finger and wrist flexion was preserved with a most satisfactory grip strength. The 2 short incisions of the fascia lata harvesting procedure healed uneventfully, and there was no muscle bulge noticed. No gait disturbance was identified. The patient achieved a low Disabilities of the Arm, Shoulder, Hand (DASH) score (20), returned to his work and daily activities, and was very satisfied overall (Figures 6 and 7, Video).

Figure 6. Wrist flexion and extension, 3 months after the final reconstructive procedure.
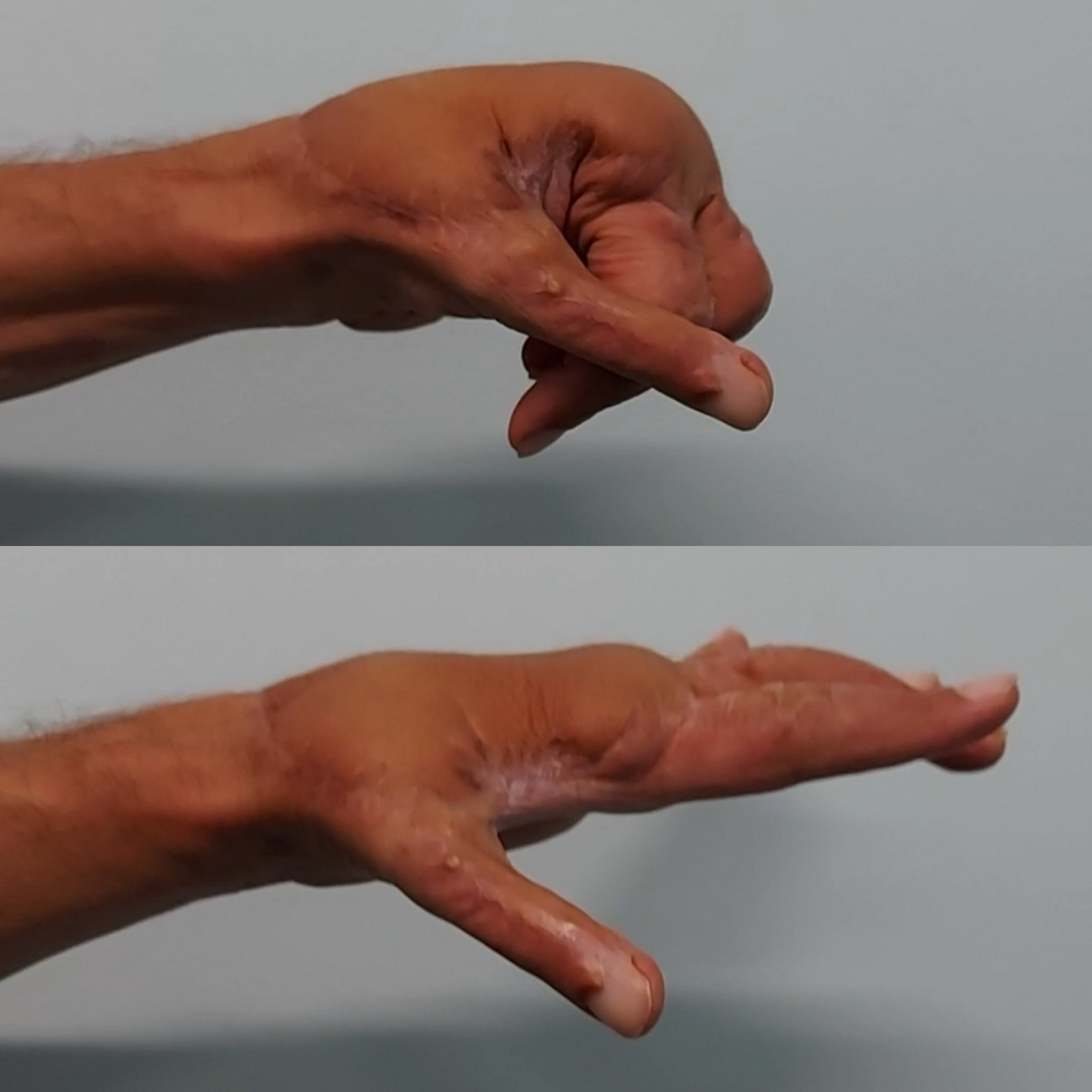
Figure 7. Finger flexion and extension, 3 months after the final reconstructive procedure.
Video. Wrist and fingers active flexion and extension, 3 months after the final reconstructive procedure
Discussion
Injuries of the dorsum of the hand and the extensor tendons as extensive as the ones described in this case are not common. Before our final decision on the surgical plan, we searched the literature for similar injuries and their treatment. To our knowledge, this is the case with the largest tendon gap so far described, extending from zones II to VII.
Single-stage reconstruction utilizing a composite tendino-cutaneous flap emerged as the preferable option from our literature research. The intact tendon sheath and the intrinsic blood supply provide the ideal environment for tendon healing and minimal adhesion formation. The number of surgeries is reduced, and a quicker recovery is achieved through early mobilization. The reverse radial forearm flap and the dorsalis pedis free flap are most often employed. Unfortunately, these reconstructive methods are accompanied with increased donor site complications and morbidity.1,2 Therefore, a single-stage reconstruction utilizing a fasciocutaneous flap with tendon grafts is a good alternative. Commonly used options are the free groin flap, the free lateral arm flap, or the free anterolateral thigh flap.3-5
Nevertheless, staged reconstruction is not considered to be an unviable approach and is still applied, especially in complicated cases.6-8 Despite the fact that more operations are needed and the recovery period is longer, staged reconstruction demonstrates comparable outcomes in terms of ROM and grip strength.5 In our case, we chose staged reconstruction because of the complexity of the injury. The extensive soft tissue trauma, the heavy contamination, and the raw scraped surfaces of the metacarpals increased the possibility of adhesion formation. The soft tissue repair over the phalanges was also unstable. If single-stage reconstruction was adopted, the small areas that were left to heal by secondary intention could potentially be sites of wound breakdown and tendon exposure. The estimated length of the tendon grafts was critically long and, in addition, the deroofing of the extensor compartments predisposed to bow stringing over the wrist. The pseudosynovial sheaths that are formed around silicon rods provide a smooth gliding surface along with a nutrient bed for the tendon grafts and sustain the normal axis of tendon movement. They also fairly substitute the extensors retinaculum.9
An additional factor that prompted us to use a staged approach was that the radial wrist extensors needed to be reconstructed, adding extra complexity to the procedure. As described earlier, fascia lata grafts were used in our case. The length of the required grafts as well as the donor site morbidity were the main arguments in favor of selecting fascia lata grafts. Three 20-cm long grafts were needed (length was equal to the tendon gap plus 3-4 cm for weaving). The average lengths of the plantaris and palmaris longus tendons are 30 cm and 15 cm, respectively.10 In order to obtain three 20-cm long grafts, the plantaris tendons of each lower extremity and an additional tendon graft would be needed. In order to reduce the morbidity of multiple harvesting incisions, we chose to obtain 3 fascia lata strips. The grafts that are routinely mentioned in the literature for extensor tendon gap reconstruction are the palmaris longus tendon and strips of the flexor carpi radialis tendon for short gaps and the plantaris tendon for longer defects. The extensor indicis proprius, the extensor digiti minimi, and the extensor digitorum longus tendons of the middle and small toes have also been described.11
Allogenic tendon grafts are also an option; however, they have not gained popularity among reconstructive surgeons, presumably because of the possibility of rejection as well as of disease transmission.12 Additionally, reconstruction with synthetic tendons has been described with good reported results but has not yet expanded in use.13 Vascularized fascia lata as part of a chimeric anterolateral thigh flap has been successfully used for dorsal hand defects, combined with single-tendon reconstruction.14 On the contrary, non-vascularized fascia lata grafts are not commonly used. The outcome of the presented reconstruction (no rupture has been noted 4 years postoperatively) demonstrates their durability and efficacy. The selection of a pedicled flap vs a free flap in our case was at the time justified because of the lack of essential microsurgical equipment. Silicon rod placement was also postponed until the flap division in order to avoid an infection, given the initial heavy contamination of the wound. Finally, patient cooperation and adherence to the early physiotherapy protocols should not be underestimated. These factors maintained the ROM throughout the reconstruction phase and prevented a rupture in the early postoperative period.
Conclusions
This case demonstrated that large dorsal hand defects combined with extensive multiple extensor tendon loss can be satisfyingly reconstructed in stages with the help of silicon rods and fascia lata grafts.
Acknowledgments
Authors: Christos Gakis, MD, MSc; Ioannis Michalis, MD, MSc
Affiliation: Department of Plastic Surgery and Burns Unit, KAT General Hospital, Kifisia, Greece
Correspondence: Christos Gakis MD, MSc, Plastic Surgery Department and Burns Unit, KAT General Hospital, Nikis 2, Kifisia 145 61, Athens, Greece. E-mail: gakis_christos@yahoo.gr
Ethics: Human subjects have given informed consent for the use of images. The authors have conformed to all appropriate institutional guidelines.
Disclosures: The authors declare that they have no conflict of interest. This study was not funded.
References
- Taylor GI, Townsend P. Composite free flap and tendon transfer: an anatomical study and a clinical technique. Br J Plast Surg. 1979;32(3):170-183. doi:10.1016/0007-1226(79)90030-4
- Yajima H, Inada Y, Shono M, Tamai S. Radical forearm flap with vascularized tendons for hand reconstruction. Plast Reconstr Surg. 1996;98(2):328-333. doi:10.1097/00006534-199608000-00019
- Benhaim T, Perignon D, Qassemyar Q, et al. Couverture d'une perte de substance de la face dorsale de la main par lambeau antérolatéral de cuisse : description, cas clinique et revue de la littérature. Reconstruction of hand dorsum soft tissue defect using anterolateral thigh perforator flap: description, case study and review of literature. Chir Main. 2011;30(1):56-61. doi:10.1016/j.main.2011.01.006
- Sundine M, Scheker LR. A comparison of immediate and staged reconstruction of the dorsum of the hand. J Hand Surg Br. 1996;21(2):216-221. doi:10.1016/s0266-7681(96)80102-1
- Lies S, Horowitz A, Lee G, Zhang AY. Review of the optimal timing and technique for extensor tendon reconstruction in composite dorsal hand wounds. Plast Aesthet Res. 2019;6:18. doi:10.20517/2347-9264.2019.27
- Al-Qattan MM. Two-staged extensor tendon reconstruction for zone 6 extensor tendon loss of the fingers: indications, technique and results. J Hand Surg Eur Vol. 2015;40(3):276-280. doi:10.1177/1753193413517626
- Abdulaziz MKB, Al-Ali AB, Hassan Z, Abdelaty M, Alkandari QA, Piccolo NS. Two-stage reconstruction of hand extensor tendons using silicon rods. Plast Reconstr Surg Glob Open. 2021;9(10):e3858. doi:10.1097/GOX.0000000000003858
- Cautilli D, Schneider LH. Extensor tendon grafting on the dorsum of the hand in massive tendon loss. Hand Clin. 1995;11(3):423-429.
- Hunter JM, Jaeger SH, Matsui T, Miyaji N. The pseudosynovial sheath--its characteristics in a primate model. J Hand Surg Am. 1983;8(4):461-470. doi:10.1016/s0363-5023(83)80209-3
- Jakubietz MG, Jakubietz DF, Gruenert JG, Zahn R, Meffert RH, Jakubietz RG. Adequacy of palmaris longus and plantaris tendons for tendon grafting. J Hand Surg Am. 2011;36(4):695-698. doi:10.1016/j.jhsa.2011.01.007
- Bertolini M, Faccenda C, Parolo C, et al. Reconstruction of tendon losses. Plast Aesthet Res. 2023;10:34. doi:10.20517/2347-9264.2022.121
- Wang GH, Mao T, Xing SG, et al. Functional reconstruction of severe hand injuries using allogeneic tendons: a retrospective study. J Int Med Res. 2020;48(10):300060520955032. doi:10.1177/0300060520955032
- Abdullah S. Usage of synthetic tendons in tendon reconstruction. BMC Proc. 2015;9(Suppl 3):A68. doi:10.1186/1753-6561-9-S3-A68
- Sơn TT, Dung PTV, Thúy TTH, Nghĩa PT, Chiến VH. Using free chimeric anterolateral thigh flap for reconstruction of composite dorsal hand defect. JPRAS Open. 2023;39:106-113. doi:10.1016/j.jpra.2023.11.011