Controversy of Breast Reduction in Adolescent Patients: An Overview of a Sometimes-Challenging Proposition
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Questions
- What is the definition of adolescence, and why might an adolescent pursue reduction mammaplasty (RM)?
- What impact does RM have on a woman’s ability to breastfeed?
- What are the prevalence and impact of postoperative regrowth of the breasts following RM in adolescent patients?
- What are the predominant methods of breast reduction, and which operation would be the best choice for adolescent patients?
Case Description
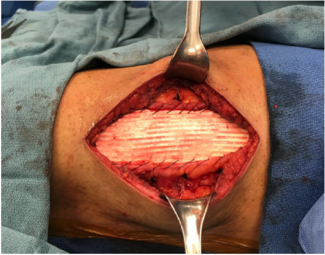
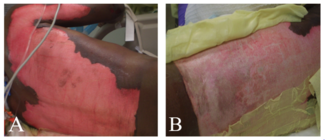
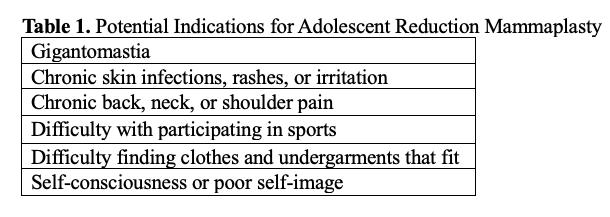
A 19-year-old woman presented to the plastic surgery department seeking bilateral RM of medical necessity after initial evaluation by a primary care physician. The patient complained of back, neck, and shoulder pain accompanied by inframammary rashes and macromastia. Upon physical examination, the patient’s left breast appeared lower and larger than the right, as shown in Figure 1. The patient had a 40I-cup bra size and no problems with her breasts other than persistent rashes and macromastia. After extensive discussion regarding the risks and benefits of the procedure, the patient chose to proceed with surgery. A right RM with the vertical technique in a superomedial pedicle was performed, and 540 g of tissue were removed. The same procedure was done on the left side with 560 g removed. The surgery was successful and resulted in excellent symmetry; intact nipple sensation; and no seroma, hematoma, or erythema. The patient was satisfied with the functional and aesthetic outcomes of the procedure. A postoperative view of the patient is provided in Figure 2.
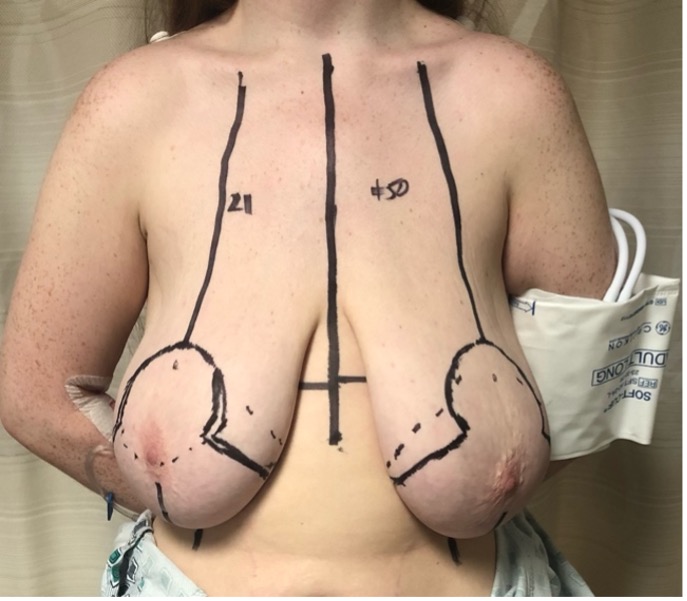
Figure 1. Image of the patient prior to reduction mammaplasty.

Figure 2. Image of the patient immediately following reduction mammaplasty.
Q1. What is the definition of adolescence, and why might an adolescent pursue RM?
RM is an established and reliable surgical procedure for adult women in need of decreased breast size for pain relief, psychological well-being, or aesthetics. However, further consideration is often warranted for adolescent women seeking RM, as the greater potential for future pregnancy(ies) must be factored into the decision to pursue surgery.1 Because the decision for therapeutic intervention might differ between patient populations with the same indications, the boundary separating adolescents from adults must be clearly demarcated. The World Health Organization and the United Nations both define adolescence as the ages between 10 and 19 years.2,3 However, recent literature has suggested that a modified age range of 10 to 24 years may be more appropriate.4,5 This range represents a population of patients impacted by a broad and dynamic array of social, economic, and corporeal health risks that are unique to adolescents.5
Advancements in education and increased access to resources at younger ages have promoted the early adoption of adult roles, thus providing steady support for the notion that adolescence begins at the end of the first decade.5 In contrast, however, the suggested age for the beginning of adulthood has risen substantially in recent times, largely because of the pursuit of higher education, changing economic factors associated with having children, shifts in social norms surrounding marriage and childbearing, and the availability of effective contraception.6 Furthermore, children commonly remain as dependents on their parents’ health insurance plans until they are 26 years old.
Determining the age of adolescence is particularly important when identifying appropriate populations for RM because of the associated risks and complications of the procedure. Redefining adolescence as between ages 10 and 24 years would include older patients who are more inclined to pursue RM because of increased breast development. Thus, as the literature shifts toward using an extended age range to define adolescence, there is an increasingly greater demand for surgeons to appropriately assess the indications for RM. As adolescence is redefined, it is important for surgeons to engage in preoperative discussions with younger patients in order to understand their goals for future pregnancy(ies) and ensure that RM is an appropriate treatment. Notably, the reasons for pursuing RM are the same for adolescents as those for adult women.1 Shared indications between the 2 patient populations provide sufficient reason to consider RM for treatment, even in the younger patient population. Because adolescents are susceptible to the physical and psychological perturbations of a changing breast morphology, it is crucial for surgeons to determine the need for RM on a case-by-case basis for these patients. A list of potential indications for RM in adolescents can be seen in Table 1.
Q2. What impact does RM have on a woman’s ability to breastfeed?
Positive effects on physical and psychosocial well-being have been observed following RM in adolescents.7,8 However, the potential contraindications of RM in this demographic must also be recognized. Because definitions regarding the ability to breastfeed are not uniform across studies, there is a lack of homogenous data, and, as a result, the impact of RM on breastfeeding ability is widely contested in the literature.9 According to meta-analysis, however, the data indicates that women who have undergone RM were 3.5 times less likely than control subjects to be physiologically capable of breastfeeding.9 This is concerning because, in 2022, nearly 6000 breast reductions were performed on patients 19 years or younger.10
Lack of education, support, and/or encouragement from medical staff are often cited as primary reasons why women who undergo RM are less likely to breastfeed.11 These are provisions that should be available to all patients, regardless of surgical history. However, given the albeit incongruent data, women who undergo RM may receive additional benefit from these services.
Q3. What are the prevalence and impact of postoperative regrowth of the breasts following RM in adolescent patients?
One major consideration in the decision to either pursue or delay RM in adolescents is the possibility of postoperative regrowth of the breasts—an occurrence that may negate the positive effects of the procedure.7 Postoperative regrowth is problematic, as secondary operations are complex, challenging, and have significantly higher rates of complications.12 Meta-analysis of the available literature indicated that 18% of adolescents experienced regrowth of their breasts postoperatively, and 2.7% of patients received a secondary mammaplasty.13 Post-operation, adolescents may continue to grow, are likely to gain weight as they age, and may experience changes in breast size or shape because of future pregnancy or breastfeeding. Consequently, some parents and surgeons may be inclined to delay breast reduction.7
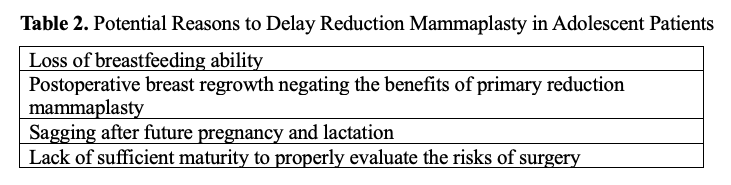
Though there are risks associated with any operation, there is considerable debate as to the degree of risk posed to adolescents undergoing RM. However, despite the risk, the guidelines set forth by the American Society of Plastic Surgeons indicate that—as long as the adolescent is the party to initiate the surgical consultation, possesses sufficient maturity, and holds realistic goals—the adolescent should be granted the opportunity to discuss RM as treatment for macromastia.14 As with any procedure, it is important to ensure that adolescents pursuing RM are informed of the potential risks prior to providing consent to treatment. A list of reasons to potentially delay breast reduction in adolescent patients is displayed in Table 2.
Q4. What are the predominant methods of breast reduction, and which operation would be the best choice for adolescent patients?
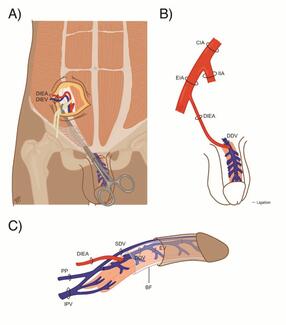
When the nipple-areolar complex (NAC) is stimulated, increased secretion of prolactin and oxytocin drives milk production. The milk then travels from the mammary lobules, through the milk ductules and ducts, and into the sub-areolar reservoirs where the milk is then secreted through the nipple.15 As long as the sensitivity of the NAC and the underlying parenchyma are sufficiently preserved, breastfeeding after reduction mammaplasty should be possible.11 Thus, the ideal method of breast reduction in adolescents is the one that most effectively spares nipple sensitivity and the underlying parenchyma.
In order to preserve nipple sensitivity and subsequent breastfeeding ability, the nerve supply to the NAC must remain intact. This requires the employment of a dermal pedicle, defined as a strip of skin within which lies the neurovascular supply to the NAC. The pedicles can extend in any direction, and breast reduction techniques are based upon in which direction the pedicle lies.16
There is considerable debate about which pedicle is the most effective at preserving lactation. According to meta-analysis, the data regarding the medial, horizontal, vertical, and central pedicle techniques are inconclusive.9 Conclusions can, however, be drawn about the lateral, inferior, and superior pedicles. The data indicate that successful breastfeeding is likely to occur in 64% of inferior pedicle patients, 59% of superior pedicle patients, and 55% of lateral pedicle patients, while the overall breastfeeding success rate following RM is 62%.9 More research is required to determine the breastfeeding success rates of patients who receive medial, horizontal, vertical, or central pedicles, as significant data regarding these techniques are lacking.9
Despite a lack of published data, the central pedicle technique is—in theory—a promising option for future breast reductions in adolescents. The conical nature of the procedure allows for maximal preservation of the glandular tissue and neurovasculature between the nipple and the chest wall.17 Therefore, breastfeeding ability should be spared with this technique. As of 2023, only 2 studies have assessed breastfeeding ability following RM with a central pedicle. In both studies, however, high success rates were reported, with 1 study reporting 100% success and the other showing 98%.9,17,18 Though these results are promising, further publications are necessary to determine the efficacy of this technique in adolescents.
The limitation of the inferior and central pedicle techniques when performed on adolescents is the reduced blood supply, as dermal continuity around the NAC must be preserved if a secondary RM is desired. Reduced blood supply poses the risk of NAC necrosis, possibly necessitating further surgical intervention.12
Acknowledgments
Authors: Quinton L. Carr, BA1; Sierra Shockley, MS1; Colton Connor, BS1; Shriya Dodwani, BA1; Claire Fell, BS1; Ryan Cantrell, BS1; Wilson Huett, MD2; Bradon J. Wilhelmi, MD2
Affiliations: 1University of Louisville School of Medicine, Louisville, Kentucky; 2Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Louisville, Louisville, Kentucky
Correspondence: Bradon J. Wilhelmi, MD, Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Louisville, 550 South Jackson Street, ACB 2nd Floor, Louisville, KY 40202, USA. E-mail: bradon.wilhelmi@louisville.edu
Ethics: The patients in this document have been provided informed consent on the use of their images and granted the use of their images for scientific publications.
Sources of Support: None
Disclosures:The authors disclose no relevant financial or nonfinancial interests.
References
1. Aillet S, Watier E, Chevrier S, Pailheret JP, Grall JY. Breast feeding after reduction mammaplasty performed during adolescence. Eur J Obstet Gynecol Reprod Biol. Feb 10 2002;101(1):79-82. doi:10.1016/s0301-2115(01)00517-6
2. Organization WH. Adolescent Health. Accessed June 26, 2024, https://www.who.int/health-topics/adolescent-health/#tab=tab_1
3. (UNICEF) UNICsEF. Adolescence. Accessed June 26, 2024, https://www.unicef.org/adolescence
4. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. Mar 2018;2(3):223-228. doi:10.1016/s2352-4642(18)30022-1
5. Kinghorn A, Shanaube K, Toska E, Cluver L, Bekker LG. Defining adolescence: priorities from a global health perspective. Lancet Child Adolesc Health. May 2018;2(5):e10. doi:10.1016/S2352-4642(18)30096-8
6. Patton GC, Olsson CA, Skirbekk V, et al. Adolescence and the next generation. Nature. Feb 21 2018;554(7693):458-466. doi:10.1038/nature25759
7. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and Quality of Life following Reduction Mammaplasty in Adolescents and Young Women. Plast Reconstr Surg. Sep 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
8. Nguyen JT, Palladino H, Sonnema AJ, Petty PM. Long-term satisfaction of reduction mammaplasty for bilateral symptomatic macromastia in younger patients. J Adolesc Health. Jul 2013;53(1):112-7. doi:10.1016/j.jadohealth.2013.01.025
9. Koussayer B, Taylor J, Warner J, et al. Breastfeeding Ability After Breast Reductions: What does the Literature Tell us in 2023? Aesthetic Plast Surg. Mar 2024;48(6):1142-1155. doi:10.1007/s00266-023-03690-8
10. Briefing Paper: Plastic Surgery for Teenagers. American Society of Plastic Surgeons. Accessed September 11, 2024, 2024. https://www.plasticsurgery.org/news/briefing-papers/briefing-paper-plastic-surgery-for-teenagers
11. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: Systematic review of observational studies. PLOS ONE. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
12. Broer PN, Moellhoff N, Aung T, et al. How to Approach Secondary Breast Reduction: International Trends and a Systematic Review of the Literature. Aesthetic Plastic Surgery. 2021;45(6):2555-2567. doi:10.1007/s00266-021-02243-1
13. Hudson AS, Morzycki AD, Guilfoyle R. Reduction Mammaplasty for Macromastia in Adolescents: A Systematic Review and Pooled Analysis. Plast Reconstr Surg. Jul 1 2021;148(1):31-43. doi:10.1097/PRS.0000000000008102
14. Policy Statement: Breast Augmentation in Teenagers. American Society of Plastic Surgeons. Accessed 9/16/2024, 2024. https://www.plasticsurgery.org/documents/Health-Policy/Positions/policy-statement_breast-augmentation-in-teenagers.pdf
15. Chiummariello S, Cigna E, Buccheri EM, Dessy LA, Alfano C, Scuderi N. Breastfeeding after reduction mammaplasty using different techniques. Aesthetic Plast Surg. Mar 2008;32(2):294-7. doi:10.1007/s00266-007-9023-8
16. Hall-Findlay EJ, Shestak KC. Breast Reduction. Plast Reconstr Surg. Oct 2015;136(4):531e-544e. doi:10.1097/prs.0000000000001622
17. Copcu E. A versatile breast reduction technique: conical plicated central U shaped (COPCUs) mammaplasty. Ann Surg Innov Res. Jul 3 2009;3:7. doi:10.1186/1750-1164-3-7
18. Sinno H, Botros E, Moufarrege R. The effects of Moufarrege total posterior pedicle reduction mammaplasty on breastfeeding: a review of 931 cases. Aesthet Surg J. Sep 1 2013;33(7):1002-7. doi:10.1177/1090820x13501857