Batwing Mammoplasty Modification as a Treatment for Hurley Stage III Breast Hidradenitis Suppurativa
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Questions
1. What is the prevalence of breast hidradenitis suppurativa (HS) and what are the indications for wide surgical excision of breast HS?
2. What surgical treatment strategies for breast HS have been previously described in the published literature?
3. What is the batwing mammoplasty modification?
4. How does the modified batwing reduction mammoplasty technique address the need for wide excision of HS disease while preserving breast aesthetics in patients with concurrent severe HS and macromastia?
Case Description
A 31-year-old woman with a history of Crohn's disease, arthritis, obesity (BMI 48.2 kg/m2), and macromastia presented with painful Hurley stage III hidradenitis suppurativa (HS), affecting her upper abdomen, 50% of both breasts, and the nipple areolar complex (NAC) of the left breast. The patient was offered a complete mastectomy with primary closure or a wide local excision of the HS with closure of the defect using an adjacent tissue transfer technique. Given the extensive involvement of the NAC with the HS, the patient was not interested in an attempted salvage and was offered 3-dimensional nipple tattooing.
She therefore elected to undergo the batwing mammoplasty modification procedure, allowing for complete excision of the HS disease while preserving the upper-pole fullness she desired. The patient developed a small seroma postoperatively that did not require surgical intervention. The patient otherwise recovered with no complications and was satisfied with her contour; she has not had any disease recurrence.
Q1. What is the prevalence of breast hidradenitis suppurativa (HS) and what are the indications for wide surgical excision of breast HS?
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory disorder primarily affecting opposing skin surfaces in areas such as the axillary, inframammary, gluteal, inguinal, and perineal regions.1 It is a highly morbid disease that negatively impacts quality of life because of significant pain, odor, extensive scarring, and cosmetic stigmatization.2 The severity of HS is classified by the Hurley staging system; stage I is the lowest grade and manifests as painful inflamed nodules or abscesses. Disease progression can lead to Hurley stage III, which describes widespread disease with scarring and sinus tract and fistula formation in multiple areas of the body.3 In the literature, the overall prevalence of HS is 0.1% to 4.1% in the general population,2 and the reported prevalence of breast HS is between 16.4% to 25.9% of HS cases in the literature.4-6
HS treatment requires a multimodal approach based on the stage of disease. Stage I treatment includes antibiotics and hygiene changes as preventative measures for disease progression. Higher stage HS treatment uses hormonal, immune-modulating, and long-term antibiotic therapies to treat more severe symptoms.7,8 In severe cases, such as Hurley stage III HS, surgical intervention in the form of wide excision is generally considered the best option because of a lower recurrence rate and higher patient satisfaction7; in the literature, disease recurrence is reported to be 27% following deroofing, 22% following local excision, and 13% following wide excision.8,9 In summary, wide excision of breast HS is indicated for severe disease or significant disease refractory to medical management and requires meticulous planning to ensure both complete disease excision and favorable breast cosmesis.
Q2. What surgical treatment strategies for breast HS have been previously described in the published literature?
Cases of breast and inframammary HS are rare and difficult to treat. There have been few case reports published on the management of breast and inframammary HS, only 2 of which describe NAC involvement.10,11 Moosa et al described their aggressive treatment by performing bilateral radical mastectomies; though this procedure was curative for HS disease of the breast, the breasts were not preserved.10 In 2004, Li et al successfully treated a patient with HS of the bilateral breasts and NAC;11 the authors performed serial excisions, debridement, allografting, and split-thickness skin grafting in 3 sessions over 5 days, preserving breast contour. A 2010 report by Nakanishi et al details the use of a Wise-pattern breast reduction for excision.9
Q3. What is the batwing mammoplasty modification?
The batwing mammoplasty modification employs a modified Wise-pattern technique (initially described by Robert Wise in 1956), which was pioneered by Christopher R. Babycos, MD, in cases of gigantomastia to help achieve better breast shape and projection and minimize necrosis. This technique utilizes a deepithelialized flap that is split into right and left halves, which are rotated underneath the upper pole to create breast projection.
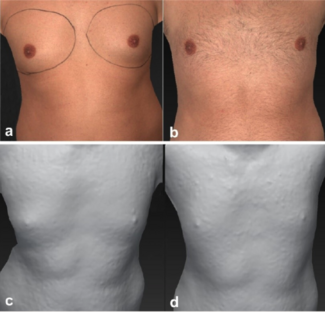
In our case, Wise-pattern preoperative markings were used (Figure 1A). The inferior incision mark was extended past the inframammary fold (IMF) to allow for excision of the HS disease on the upper abdomen and fasciocutaneous advancement of the tissue to recreate the IMF (Figure 2A and B). Two vertical lines measuring 10 to 20 cm were traced caudally (Figure 1A, “Y”), with a semicircular curve in the center to avoid the NAC. The pedicle width was set to 12 cm.
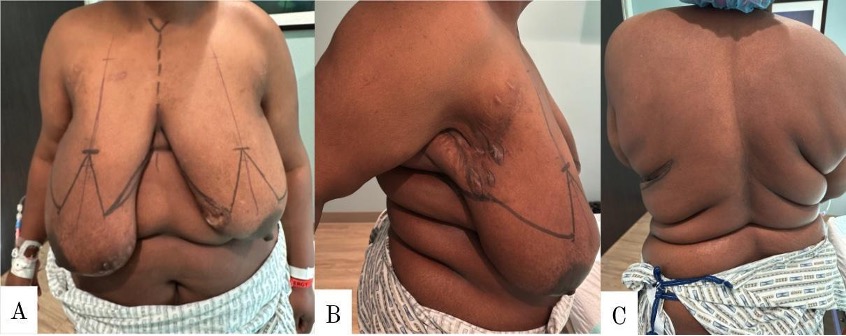
Figure 1. (A) Anterior view showing the preoperative Wise-pattern and batwing markings. X indicates the set width (8-10 cm), drawn no closer than 1 cm to the nipple. The Y marking indicates the projection-determining limb (10-20 cm). Z indicates the vertical limb of the Wise pattern. (B) Superior view of the Wise-pattern technique showing split pedicle modification. IMF = inframammary fold.

Figure 2. (A) Preoperative markings and anterior hidradenitis suppurativa disease involvement. (B) Right-side preoperative markings and axillary disease involvement. (C) Posterior disease involvement on the left flank.
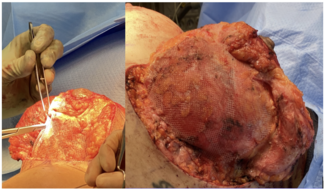
The batwing was first deepithelialized. The remainder of the Wise-pattern markings were incised, and electrocautery was used to dissect the underlying muscle fascia. The medial and lateral edges of the batwing were cut using electrocautery. An approximately 1- to 2-cm dissection was made, marking the thickness of the batwing flap. The IMF incision, carried down to muscle fascia, was continued in this plane superiorly toward the clavicle. The batwing flap was cut superiorly toward the clavicle and once the 2 dissections met, the HS affected breast tissue was excised; the right and left tissue weighed 947 g and 546 g, respectively (Figure 3B and C). To allow for inset, a full-thickness incision was made down the middle of the flap to create 2 halves (Figure 1B). Each half was then rotated underneath the breast flap (Video) and inset to the pectoralis fascia superiorly using polydioxanone sutures; this was performed until the contour of the breasts was satisfactory. The breasts were then closed in 3 layers. Iodoform wicks were placed between the sutures to allow for drainage. Blake drains were also placed (Figure 4).

Figure 3. (A) Intraoperative and (B) excised tissue with disease involvement and the nipple-areolar complex (NAC). (C) Excised tissue with disease involvement and the NAC.
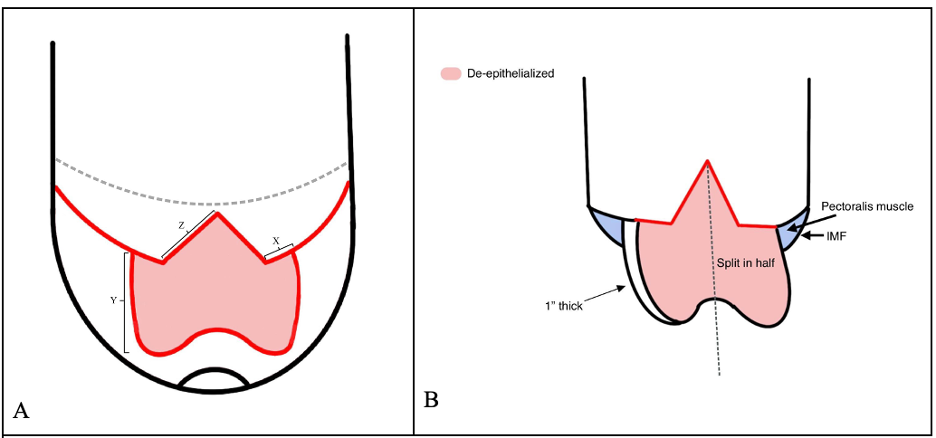
Figure 4. Anterior view of the intraoperative closure.
Q4. How does the modified batwing reduction mammoplasty technique address the need for wide excision of HS disease while preserving breast aesthetics in patients with concurrent severe HS and macromastia?
The Wise pattern is the most used skin reduction technique in breast reduction surgery, allowing for removal of vertical and horizontal skin excess.12 Compared with other excision patterns such as vertical or periareolar approaches utilized in reduction mammoplasty, the Wise (inverted T) pattern allows for the greatest amount of skin removal and has also been found beneficial in patients with poor skin quality.13 In severe or Hurley stage III HS, complete excision of the disease-affected skin is paramount; therefore, employing a skin excision pattern that allows for the widest possible resection is crucial.
Because the Wise pattern allows for resection of both vertical and horizontal skin to allow for the appropriate removal of diseased skin and can accomodate large-volume breast reduction, in comparison with other techniques, it provides a dual benefit for patients with HS. Beyond removal of the disease skin, the Wise-pattern reduction mammoplasty allows for substantial reduction in breast volume and, subsequently, the removal or reduction of the intertriginous area at the IMF known to perpetuate diseases, especially in patients with comorbid macromastia or gigantomastia.
Splitting the deepithelialized pedicle into right and left components allows for greater flexibility in shaping the breast, while preserving or enhancing upper-pole projection. The modified batwing mammoplasty gives the surgeon increased control over the final breast contour, which can help to achieve shape near the natural breast by maintaining some of the desired volume, especially in the upper pole. This supports an aesthetically pleasing result, potentially bolstering patient satisfaction and quality of life.
In summary, the modified batwing mammoplasty provides a dual benefit by addressing HS disease through wide skin excision and significant breast volume reduction, while the split deepithelialized pedicle gives the surgeon more control to optimize the breast shape in the setting of concurrent HS and macromastia.
Acknowledgments
Authors: Tatjana Mortell, BS1; Jared Rosbrugh, MS1; William Aukerman, MD2; Kevin Kresofsky, MD2; Chris Babycos, MD3; Abigail Chaffin, MD, FACS, CWSP, MAPWCA2
Affiliations: 1Tulane University School of Medicine, New Orleans, Louisiana; 2Division of Plastic and Reconstructive Surgery, Department of Surgery, Tulane University School of Medicine, New Orleans, Louisiana; 3Department of Plastic and Reconstructive Surgery, Ochsner Clinic Foundation, New Orleans, Louisiana.
Correspondence: Abigail Chaffin MD, FACS, CWSP, MAPWCA, Division of Plastic and Reconstructive Surgery, Department of Surgery, Tulane University School of Medicine, New Orleans, LA 70112, USA. E-mail: achaffin@tulane.edu
Ethics: Written informed consent was obtained from both patients for the publication of this report.
Disclosures: The authors disclose no relevant financial or other conflicts of interest.
References
- Sabat R, Jemec GBE, Matusiak Ł, Kimball AB, Prens E, Wolk K. Hidradenitis suppurativa. Nat Rev Dis Primers. 2020;6(1):18. doi:10.1038/s41572-020-0149-1
-
Scholl L, Schneider-Burrus S, Fritz B, Sabat R, Bechara FG. The impact of surgical interventions on the psychosocial well-being of patients with hidradenitis suppurativa. J Dtsch Dermatol Ges. 2023;21(2):131-139. doi:10.1111/ddg.14934
-
Posch C, Monshi B, Quint T, Vujic I, Lilgenau N, Rappersberger K. The role of wide local excision for the treatment of severe hidradenitis suppurativa (Hurley grade III): retrospective analysis of 74 patients. J Am Acad Dermatol. 2017;77(1):123-129.e5. doi:10.1016/j.jaad.2017.01.055
-
Katoulis AC, Liakou AI, Rotsiamis N, et al. Descriptive epidemiology of hidradenitis suppurativa in Greece: a study of 152 cases. Skin Appendage Disord. 2017;3(4):197-201. doi:10.1159/000475822
-
Shih T, Seivright JR, McKenzie SA, et al. Gender differences in hidradenitis suppurativa characteristics: a retrospective cohort analysis. Int J Womens Dermatol. 2021;7(5 Pt B):672-674. doi:10.1016/j.ijwd.2021.07.003
-
Díaz D, Rivera A, Otero V, Rueda L. Epidemiology of hidradenitis suppurativa: current status. Curr Dermatol Rep. 2022;11(4):336-340. doi:10.1007/s13671-022-00372-7
-
Kolli SS, Pona A, Cline A, Marks M, Feldman SR, Pichardo RO. Surgical options in hidradenitis suppurativa. Journal of Dermatology & Dermatologic Surgery. 2019;23(1):2-6. doi:10.4103/jdds.jdds_35_18
-
Shukla R, Karagaiah P, Patil A, et al. Surgical treatment in hidradenitis suppurativa. J Clin Med. 2022;11(9):2311. doi:10.3390/jcm11092311
-
Nakanishi M, Yokota K, Ochi M. Surgical management of hidradenitis suppurativa in the sub-mammary area. J Plast Reconstr Aesthet Surg. 2010;63(2):e177-e179. doi:10.1016/j.bjps.2009.01.084
-
Moosa HH, McAuley CE, Ramasastry SS. Surgical management of severe mammary hidradenitis suppurativa. Ann Plast Surg. 1988;20(1):82-85. doi:10.1097/00000637-198801000-00013
-
Li EN, Mofid MM, Goldberg NH, Silverman RP. Surgical management of hidradenitis suppurativa of the nipple-areolar complex. Ann Plast Surg. 2004;52(2):220-223. doi:10.1097/01.SAP.0000070641.63963.75
-
Ali AOM, El-Wahab EHA, Othman AG, Essam AERM. Comparison between batwing versus Wise pattern mammoplasty for upper pole breast tumors. Medical Journal of Cairo University. 2021;89(2):569-584. doi:10.21608/mjcu.2021.167850
-
Wong C, Vucovich M, Rohrich RJ. Mastopexy and reduction mammoplasty pedicles and skin resection patterns. Plast Reconstr Surg Glob Open. 2014;2(8):e202. doi:10.1097/GOX.0000000000000125