Clinical Summary of Placental Allograft Reconstruction of Cutaneous Wounds Following Mohs Surgery: A Propensity Score-Matched Comparative Cost-Effectiveness Analysis Advances

Clinical Summary
Dehydrated human amnion/chorion membrane (DHACM) may provide a cost-effective alternative to autologous skin flaps or grafts for reconstruction in patients undergoing Mohs micrographic surgery (MMS) in areas with elevated functional or cosmetic risk, according to a recent study by Toman et al.
DHACM allografts have previously been shown to provide positive outcomes without added costs in other wound types, including diabetic foot ulcers, and this study suggests that similar results may extend to post-MMS reconstruction.
Basal and squamous cell carcinomas, the most common types of cancer in the United States, have seen an alarming rise in occurrence in recent years. MMS is considered the preferred technique for resection of these tumors, but quality of life for patients largely depends on subsequent cutaneous reconstruction to restore form and function to the affected area, particularly in areas such as the face, scalp, and dorsal hands. Autologous tissue-based reconstructive methods have been the standard of care (SOC) for post-MMS reconstruction, but this study sought to assess whether a placental allograft could provide equal or better results at a similar overall cost.
The retrospective comparative cohort study evaluated the average cost and effectiveness of DHACM (EPIFIX; MIMEDX Group, Inc) compared with SOC (skin flaps and autologous skin grafts), focusing on defects in areas with functional or cosmetic risk that could not be closed primarily. By querying administrative practice databases for patients who underwent MMS with same-day reconstruction between 2014 and 2018, authors compiled a final cohort of 429 subjects who met all inclusion criteria and were then evaluated using a propensity-score-matching model, matching a subject receiving EPIFIX with an autologous tissue control in a 1:2 case-control ratio.
After comparing the 143 DHACM subjects against the 286 control subjects, researchers noted that DHACM was more expensive than SOC in the primary reconstruction phase. However, post-repair sequelae costs for the test group were notably lower than those in the SOC group due to significantly fewer adverse events. Specifically, adverse post-repair sequelae occurred in just 2.3% of patients receiving EPIFIX but 21.3% of patients treated with autologous tissue. Rates of dehiscence, flap or graft necrosis, and hematoma were all significantly lower in the DHACM group, where patients also had fewer surgical revisions and achieved their final disposition at a faster rate, with an average length of care of 33.3 days, compared with 48.3 days for control patients. As such, there was no significant difference in cumulative costs found between the 2 cohorts.
Complication Comparison for DHACM and Autologous Tissue Following MMS
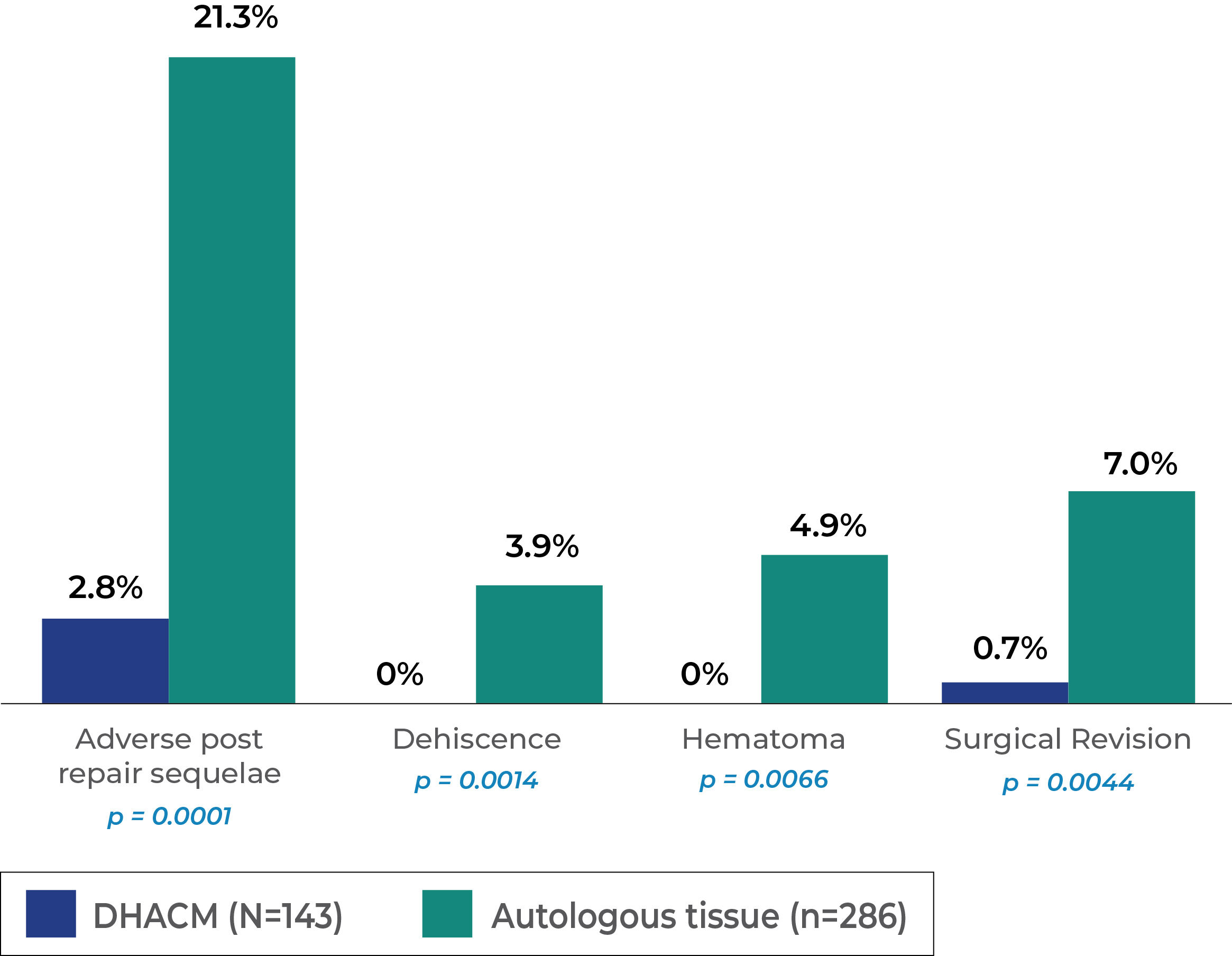
Adverse post-repair sequelae occurring in this study population.
Overall, the authors noted that the purchase of the placental allografts accounted for 76.4% of total reconstruction costs, on average, as treatment with DHACM helped patients avoid the costs of postoperative complications. While the SOC cohort was less costly in the initial phase, the monetary costs of adverse sequelae, outpatient visits, aesthetic services, etc, not to mention the impact on patient quality of life, offset any upfront savings. For the DHACM cohort, those with defects in areas with functional or cosmetic risk, the "data suggests that in elderly patients with wounds that cannot be closed primarily, DHACM appears to be a useful alternative to standard skin grafting and skin flaps with minimal financial tradeoff." The authors conclude, recommending a placental allograft such as EPIFIX be particularly considered in cases of larger defects (>3.0 cm) in moderate to high risk, functionally and cosmetically sensitive areas.
Reference: