Mountain View Paramedic Institute Flipped EMS Education on its Head
Have you ever marveled at how one paramedic can walk into a room and, within 60 seconds, deduce whether a patient’s life is threatened while immediately intuiting an appropriate application of diagnostics and developing a logical and likely treatment plan in the back of their mind? At the same time, another medic feels hamstrung, waiting until diagnostics have been tested and evaluated before acting on the patient’s behalf. The stark difference between these types of medics may be attributed to the way they acquired their knowledge and skills, as well as their level of engagement in the learning process. This article and accompanying video essay examine and support the notion that revolutionizing paramedics' learning will improve their retention, performance, and patient outcomes.
Learning is a lifelong process, but educators who teach students in high-stakes fields like paramedicine know that the way learning happens can make a lifesaving difference. Traditional classroom models, based on a lecture followed by homework, often fall short in preparing students for the fast-paced, critical thinking demands of the job.

In the pursuit of graduating well-informed and well-prepared paramedics, the Mountain View Hospital Paramedic Institute, located on-property at Mountain View Hospital in Las Vegas, Nevada, flipped the traditional learning model “on its head.” By embracing the flipped classroom approach to paramedic education, the program’s leaders challenge the passive "listen and learn" method and replace it with empowered engagement where students take control of their own knowledge. The result?
We are producing a new generation of paramedics who are not just memorizing facts but are actively applying them in the classroom before they ever step into the field.
Understanding the "Flipped" Approach
“A flipped classroom inverts the traditional learning model, with students completing foundational learning (video lectures, readings, etc.) at home, and then subsequently engaging in hands-on practice,” said the Institute’s academic director, Nicole Brown, EdD, MSL, paramedic. “Our flipped classroom is more than just a different schedule; it's a different philosophy. This method allows students to learn at their own pace and come to class prepared to dive deeper into the subject matter through interactive and applied learning experiences."
The focus on active learning is designed to enhance student engagement and ensure information sticks, which is crucial for a field in which every second counts.
Each week, students attend scheduled labs that include the following:
- Teach-backs: Students are assigned to present the homework information to their peers using lectures, a game, a puzzle, etc.
- Scenario Testing: Students participate in scenario testing with a small group and an instructor/preceptor.
- Skills practice/treatment planning: Students work together in small groups, collaborating in skills practice and treatment planning.
- MCI/Disaster Drills: Annually, the program’s lab session includes a community-wide MCI/disaster drill.
- Clinical Rotations: The institute is considered one of Mountain View Hospital’s teaching/residency programs. Students rotate and apply their skills across all hospital departments, including Labor and Delivery, Pediatrics, ICU, CCU, and the Emergency Department.
The Value of Guest Lecturers
The program uses a wide array of expert guest lecturers to keep the education fresh and relevant. These lectures offer students valuable insights and networking opportunities with hospital staff members. The program extends invitations to its network of guest lecturers. From interventional radiologists discussing stroke care to trauma surgeons sharing what they need from EMS providers, these experts bring their real-world experience to the classroom.
"We cannot match the education provided by guest lecturers," Brown said. "We can come close, but not with the same flair."
Because students hear from local physicians, the process also fosters relationships that benefit students. After their presentations, anesthesiology or emergency department residents often recognize Mountain View program students when they are scheduled in the operating room or in the emergency department during the students’ clinical rotations.
The Origins of a New Model
Troy Tuke, co-founder and program director, and Suzie Kochevar, RN, MSN, co-founder and former academic manager, established the institute to address a critical shortage of paramedics in Southern Nevada in September 2019. Since its opening, the program has graduated more than 150 students. Another 60 students are currently in internship, and 65 are currently enrolled in Cohort #6.
“Susie Kochevar and I created the Mountain View Hospital Paramedic Institute specifically to help local fire and ambulance agencies fill their paramedic needs," Tuke said.
All program students have at least one year of full-time experience working as EMTs and are sponsored by a licensed EMS agency, where they continue to work ambulance shifts. Full-time employment while in paramedic school ensures that students will have an immediate opportunity to apply what they're learning through real-world experience at their respective agencies.
The program's unique educational model was inspired by the proven success of Dr. Michael Allswede, a grant-funded researcher and medical director who had previously achieved top-tier performance from his emergency medicine residents using the same active learning methods. Due to his success, Tuke and Kochevar invited Allswede to become the institute’s first medical director.
"Dr. Allswede wanted to see if we would experience the same performance results utilizing the 'flipped classroom' model for paramedic students,” Tuke said.
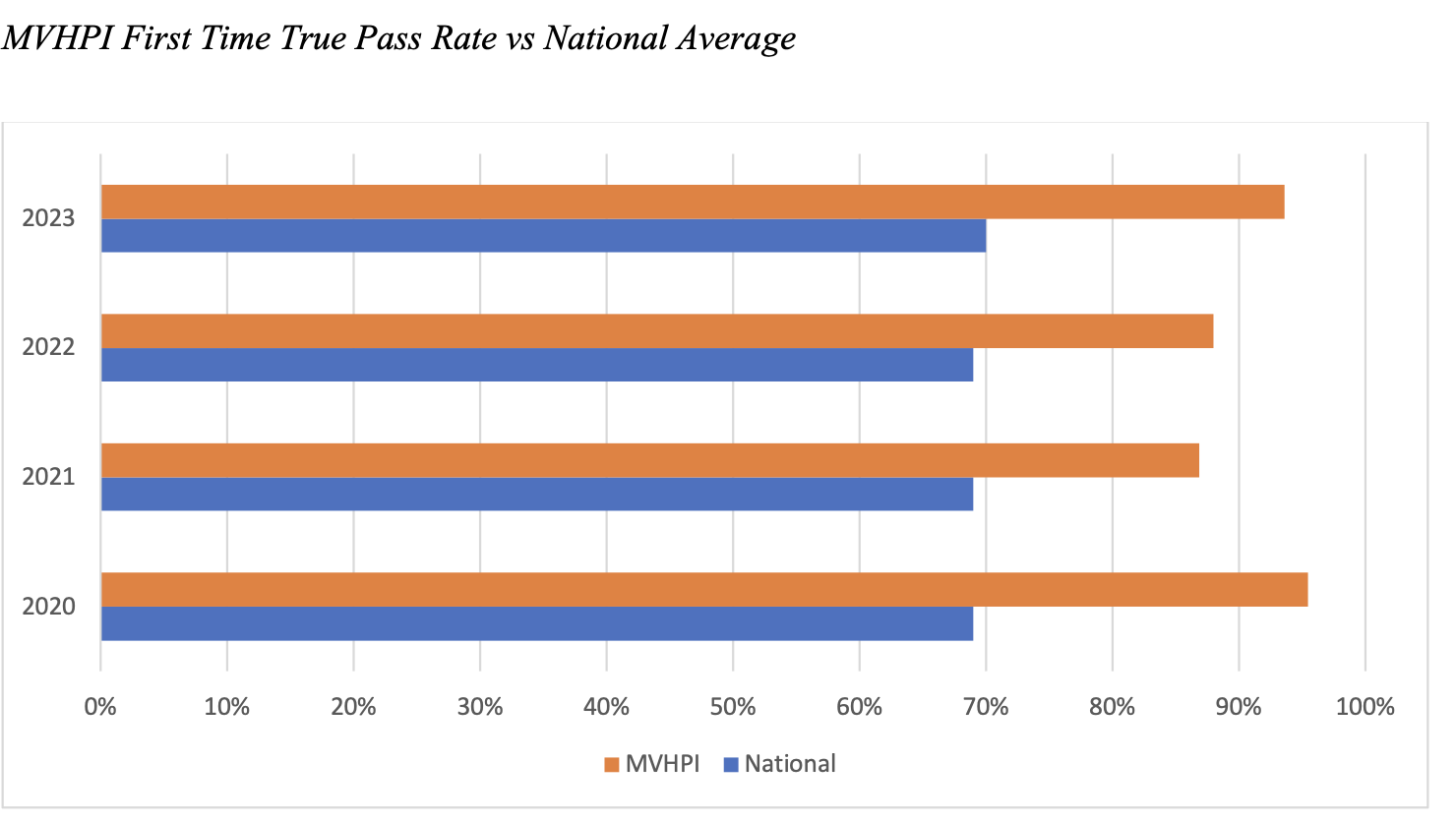
The results have been resounding, with students' test scores consistently higher than the national average.
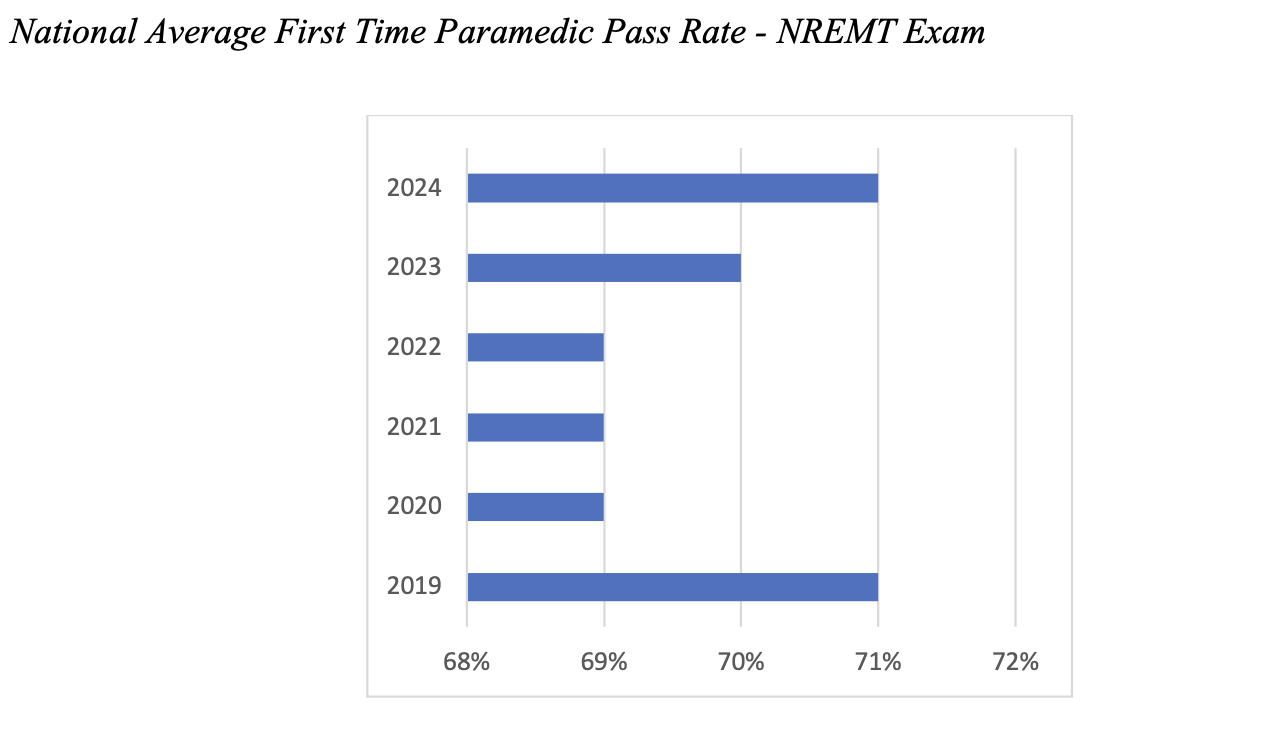
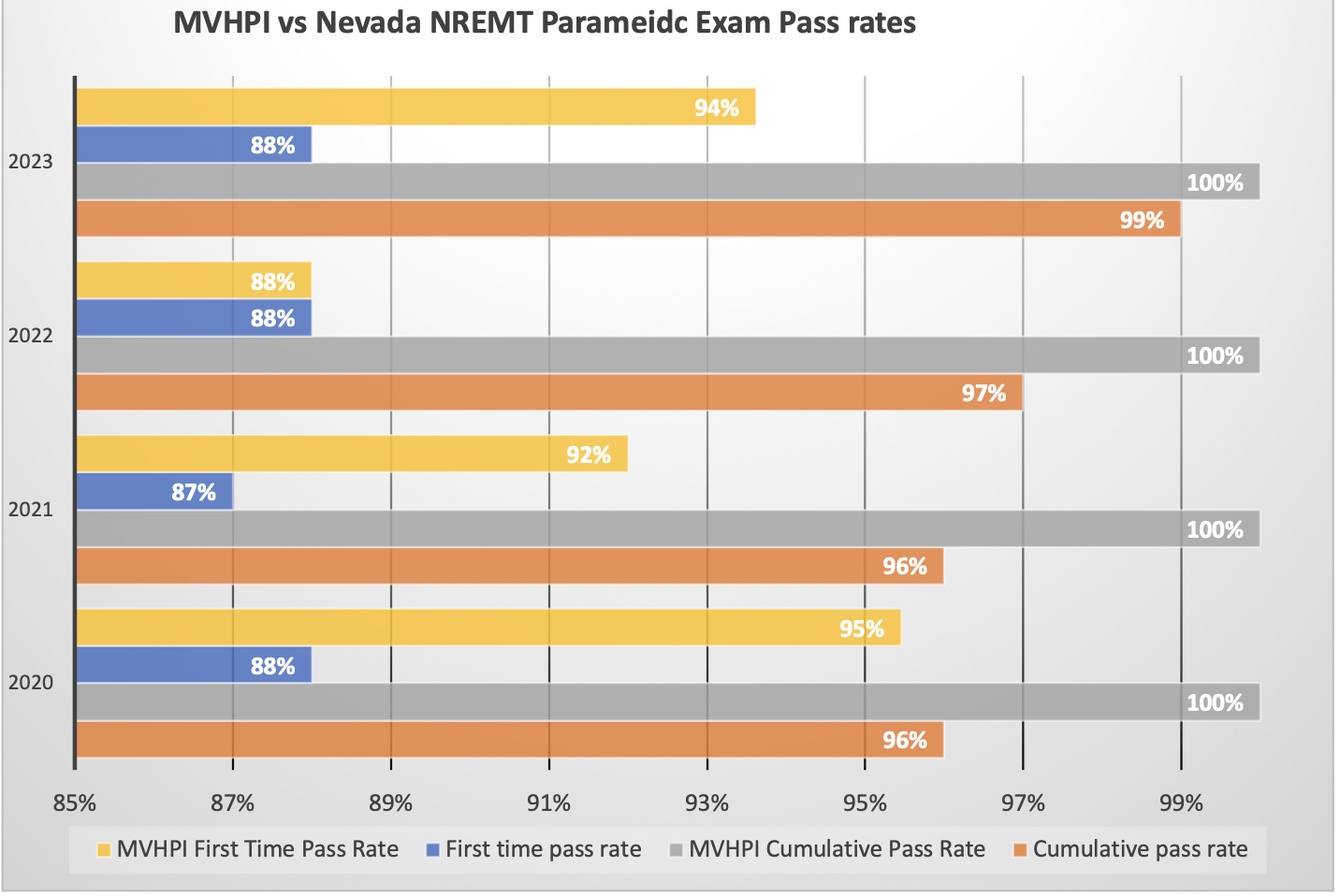
The following three graphs demonstrate the national average first-time pass rates for the National Registry’s paramedic exam, Mountain View Paramedic Institute’s pass rate in comparison to the National Registry’s average pass rates, and how the Institute’s paramedics’ pass rates compare with the State of Nevada’s average pass rate for paramedic students.
How Learning Becomes Visible
The program uses a combination of vetted unit exams and hands-on psychomotor tests to ensure that students not only retain information but also apply it accurately under pressure.
"The students always want to know what is on the test. We never review specific questions,” Brown said. “We do discuss topics and how the students would approach the situation."
This approach, she explained, is deliberate, forcing students to move beyond rote memorization. The program sets a high bar, with students needing to maintain a 75% average on all unit exams and an 80% on the final comprehensive exam.
"The students who do not achieve these markers have not invested the time and should not be put in a position to make life and death decisions,” she said.
The program also emphasizes the importance of psychomotor exams. These hands-on tests are invaluable for identifying ambivalence and ensuring that students can translate information from their brains to their hands.
The learning doesn't stop when class is over. A key component of the program is its robust clinical phase, which provides students with hands-on experience in real-world settings. Students get to apply what they've learned in ERs, operating rooms, and on field rides with their sponsoring agencies.
Proudly Delivering Confident, Competent Paramedics
The most significant source of pride for the faculty is seeing their students graduate as confident, competent paramedics who often return to the Institute to mentor future cohorts.
“Ultimately, the success of the flipped classroom model isn't just measured in test scores; it's seen in the quality of the graduates themselves,” Brown explained. “I am most proud of the paramedics who have graduated. I would trust them to care for me or my loved ones."
Local Community Support
Supporters of the Mountain View Paramedic Institute program include all EMS providers in Southern Nevada. Although the local 9-1-1 provider, Community Ambulance, accepts paramedic graduates from all paramedic teaching programs, it will only pay employees’ tuition scholarships at the Mountain View Paramedic Institute due to its proven record of producing graduates who score well above the National Registry paramedic exam and who demonstrate outstanding critical thinking skills in the field.
Standout Community Ambulance EMTs who have at least one year of experience must compete for placement at the Institute. Community Ambulance’s trust in the flipped classroom concept has grown due to the program’s track record of providing active, applied learning that prepares students for the high-pressure realities of their jobs.
“The program’s success is also evident in the intense camaraderie that develops between students who attend from all agencies, as well as the fact that many of our graduates return to the Institute to serve as preceptors and adjunct instructors, giving back to the program that has given them so much,” said Community Ambulance’s Director of Operations Mark Calabrese.
















