Mixed Messages on Medicare Cost Data Collection: Which One will Congress Hear?
The Ground Ambulance Data Collection System (GADCS) gathered information from approximately half of the ambulance service providers in the country last year, and the other half have just finished up reporting recently.
The GADCS data from the first group of reporters is in, and a summary report of that data has been published, which can be seen here: Medicare Ground Ambulance Data Collection System (GADCS) Report. From this report, it looked promising that the data would show that ground ambulance services are underpaid by Medicare.
However, this report may not be the key document upon which Congress bases their decision regarding the adequacy of Medicare payment for ambulance services.
The Medicare Payment Advisory Commission (MedPAC) is an independent congressional agency established by the Balanced Budget Act of 1997. MedPAC advises Congress on issues affecting the Medicare program. One of those issues is the sufficiency of Medicare payment schedules, and MedPAC has been tasked with summarizing the GADCS data and reporting to Congress for that purpose.
MedPAC met on March 6, 2025, to begin the initial discussion regarding ambulance cost data. A link to their full hearing can be found here: March 2025 public meeting transcript – MedPAC and the companion slides can be found here: Mandated report: Payment for ground ambulance services – MedPAC
During this initial discussion, the MedPAC committee indicated that “… the GADCS dataset is the most comprehensive dataset on ground ambulance operations. But we have some concerns about the accuracy of the data” (transcript at page 224, line 22). The first concern they note is that many ambulance organizations share costs with other entities such as fire, police, or hospitals, and MedPAC stated that these ambulance services may not have fully separated their costs from these other entities.
The other concern that MedPAC identified was that “… there are no separate variables for transports of Medicare patients or costs for Medicare patients” (see public meeting transcript beginning at page 225, line 16). They don't articulate why they believe that it may cost more, or less, to transport a patient who has Medicare as a payer than it would cost to transport a patient with the same medical condition who is uninsured or covered by commercial insurance, but they cite this as a concern nonetheless.
To alleviate these “concerns,” they have made two edits to the data. The first is that they have dropped all ambulance organizations that share costs with fire departments, police departments or hospitals. The second edit is that they have dropped all ambulance organizations that have a cost per response which are more than three standard deviations from the mean cost identified by the data (transcript at page 225, line 21, bold emphasis added by the author).
In general, when removing outliers from a sample, proper statistical sampling methodology requires that outliers not be removed unless it is certain that there is not a valid reason for their numbers to be outside of the normal range from the average, and then it is only appropriate to remove those outliers from both sides of the curve.
However, MedPAC has not articulated any rationale for why they believe ambulance services have included inappropriate fire, police, or hospital costs, and MedPAC has chosen to remove only the outliers who have significantly higher costs than the average, showing no similar concern for those organizations who might have forgotten to include certain expense and therefore have artificially lower costs, thereby skewing the data toward the lower end.
The first group of reporting ambulance agencies totaled 3,852 organizations (transcript at page 224, line 12). After the edits removing all ambulance agencies that are tied to other services and the outliers on the high end of the cost spectrum, there were only 1,710 organizations left for which MedPAC chose to recognize their data (transcript at page 226, line 11).
In other words, they removed the data from 2,142 reporting ambulance agencies, or over 55%. Ironically, the primary criticism with past Government Accountability Office (GAO) ambulance studies has been that those were too narrow and did not include sufficient data to be accurate, and now we seem to be heading down that same narrowed path again.
The impact of these edits is dramatic. Consider the following chart, which is from the original GADCS report, modified to reflect the categories of the data considered by MedPAC. The full table can be viewed in the GADCS report linked above, at page 132, Table 6.1.
| N | Mean | |
|---|---|---|
| Medicare transport volume | ||
| Low | 2,123 | $2,457 |
| Medium | 1,416 | $1,771 |
| High | 884 | $1,258 |
| Very High | 600 | $719 |
Now compare that chart to the one below, which was presented in the public meeting by MedPAC, and which represents the “edited” data.
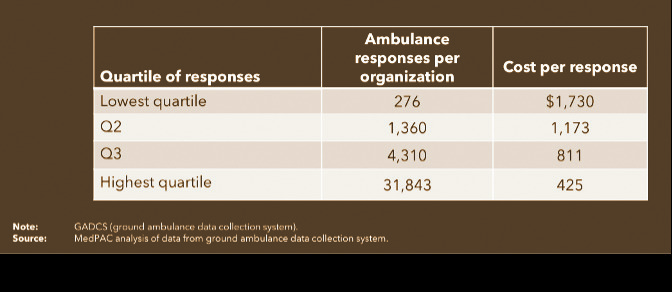
Comparing the two sets of data, after removal of more than half of the reporting agencies, the average cost of response for a low volume ambulance agency went from $2,457 in the GADCS report to $1,730 in the MedPAC presentation; a difference of $727 and a 30% reduction in estimated costs. On the other end of the spectrum, for those ambulance services with a high volume of responses, the cost went from $719 to $425; a difference of only $294, but a 41% reduction in estimated costs.
While this is the only chart that MedPAC provided in their presentation, the results of their revision of the data regarding costs are shocking. To make matters worse, the other critical piece of analysis, which is missing from their presentation, is what the adjusted revenue looks like after the removal of the majority of reporting agencies.
Keep in mind, the entire intent of this data collection project is to determine whether Medicare payments are sufficient to reimburse for the cost of providing ambulance responses and transports. Also note that while expenses per response vary greatly depending on the volume of an ambulance agency (a variance of $1,738 between high and low volume services according to the GADCS Report Table 6.1 shown above), the revenue generated does not.
From the GADCS report at page 136, Table 6.2, the average revenue per response received by a low volume ambulance service was $940 and a high-volume service was $549, a difference of only $391, most of which is probably accounted for by the rural and super-rural adjustments and longer distance transports, which include more mileage charges.
So when you consider the relatively flat rate of payment, it is unlikely that the “edits” made by MedPAC will have near as much impact on revenue as they did on costs. In other words, their adjustment to the data will have a net result of lowering costs while keeping revenue basically the same, thereby narrowing the gap between Medicare payments and the cost of providing care, and dramatically decreasing the likelihood that cost data collection will result in higher payments to the ambulance industry.
Wondering why you bothered to input all of this data, especially the 55% of you who had your data thrown out the window? I don’t blame you. And if you are one of the 700 ambulance services who did not report and are now subject to a 10% penalty on your Medicare payments, you may be paying that penalty for not reporting data that would never have been considered anyway. While that fact is a bit hard to swallow, the fact that this manipulation of the data could result in less revenue for the entire ambulance industry is a much more bitter pill.
The MedPAC public hearing transcript does note that this is only a preliminary review of the data, and the full MedPAC report to Congress is due June 15, 2026. Therefore we have a limited time to argue the validity of the entire dataset; to show that all costs included were reasonable and that there are legitimate reasons for outliers. If we do not, then we may remain underpaid by Medicare.
Legal Lesson is a regular column on regulatory matters of significance to prehospital providers by EMS World Editorial Advisory Board Member Christopher Kelly. This article is not intended as legal advice.















